The Beatles created beautiful music. John and Paul complimented each other bringing together their different styles of music to create a balance of introspection and melody. Individually, each Beatle, Ringo, Paul, John and George were great musicians in their own right, but I think it is safe to say, their collaborative work exceeded their solo work.
I am a firm believer that in health care, the best outcomes are those that are team driven. This is particularly true in complex medical conditions such as irritable bowel syndrome (IBS). 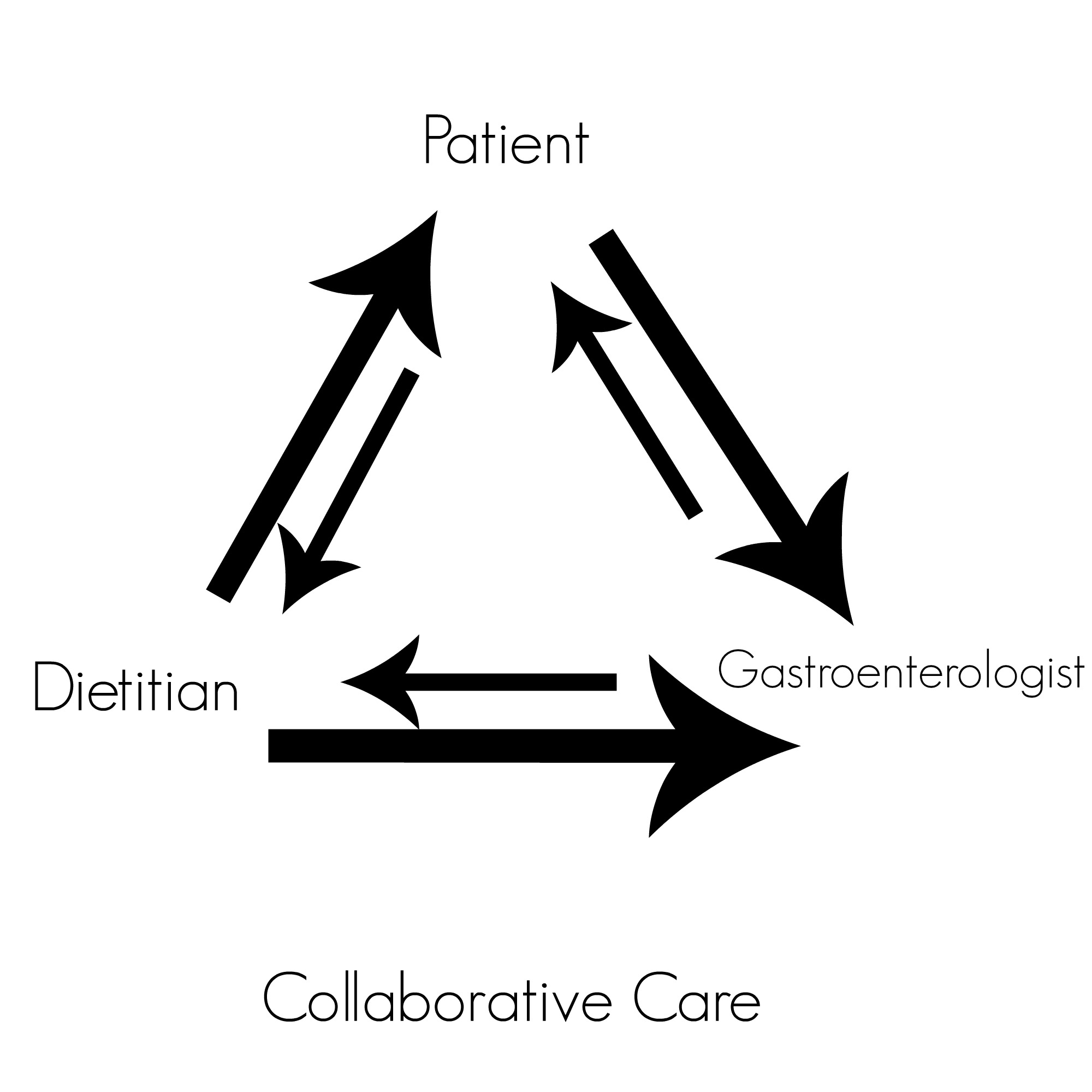 Healthcare providers often weigh in on a patient’s case from their own personal lens and expertise. As diet has been shown in research studies to help manage symptoms of IBS with better efficacy than most drugs on the market for this condition, having a dietitian working with IBS patients is paramount! Over-restricting the diet is a common occurrence in IBS patients as it can be difficult to identify personal dietary triggers, leading to potential nutritional deficiencies. There is so much misinformation on the internet, it can lead to utter confusion for the patient. The dietitian can help circumvent these issues and help maximize the nutritional well-being of the IBS patient. In my opinion, patients with complex digestive health symptoms can often benefit from a variety of providers including: gastroenterologists, pelvic floor physical therapists, providers of gut directed hypnosis, urogynecologists, allergists or immunologists, and registered dietitians to create a comprehensive treatment plan. All healthcare providers can learn from one another and together, are able to develop a comprehensive treatment plan for the best patient care.
Healthcare providers often weigh in on a patient’s case from their own personal lens and expertise. As diet has been shown in research studies to help manage symptoms of IBS with better efficacy than most drugs on the market for this condition, having a dietitian working with IBS patients is paramount! Over-restricting the diet is a common occurrence in IBS patients as it can be difficult to identify personal dietary triggers, leading to potential nutritional deficiencies. There is so much misinformation on the internet, it can lead to utter confusion for the patient. The dietitian can help circumvent these issues and help maximize the nutritional well-being of the IBS patient. In my opinion, patients with complex digestive health symptoms can often benefit from a variety of providers including: gastroenterologists, pelvic floor physical therapists, providers of gut directed hypnosis, urogynecologists, allergists or immunologists, and registered dietitians to create a comprehensive treatment plan. All healthcare providers can learn from one another and together, are able to develop a comprehensive treatment plan for the best patient care.
Do you have an IBS dream team?
I am hopeful that team driven centers will be the new approach for treatment for irritable bowel syndrome, a complex heterogenous disorder. Each patient with IBS needs to be evaluated on an individual basis as no two are alike.
A big advantage of having a dietitian involved in patient care, aside from their nutritional and medical expertise, is that their appointment time is generally a full hour or more for the initial assessment. Having this extra time with the dietitian allows the patient the time to share a very detailed summary of their symptoms. In contrast to the doctor’s limited patient time, the dietitian’s hour long visit might allow for uncovering previously unknown key pieces of the patient’s health care puzzle. I enjoy working closely with the gastroenterologist to weigh in on the patient’s case and come up with comprehensive solutions or ideas.
My hope for IBS sufferers… is that you have the opportunity to put together a collaborative team to help guide you on your path to wellness.
If you are a dietitian knowledgeable in the low FODMAP diet and digestive health be sure to reach out to your local gastroenterologists to let them know about your services. If you are a gastroenterologist, do your patients a favor and provide them a referral to a dietitian skilled in digestive health. And if you are a patient, find a skilled digestive health dietitian and gastroenterologist that work collaboratively so that you may have a comprehensive approach to getting your IBS under control.
Dr. Bill Chey of University of Michigan spoke recently at the American College of Gastroenterology’s annual conference in Hawaii speaking about role of diet in IBS and the dietitian in the treatment team.
Click here to listen.

Beth Anderson
Completely agree, but unfortunately we have a long way to go for IBS treatment in the United States. My experience is that the GI docs still do not take this condition seriously. All the medical advice out there seems to be “eat more fruits, veggies, and fiber,” “treat with anti-depressants” and “learn to manage your stress better.” I finally came across the low fodmap approach randomly on the internet. I tried the diet and it solved the problem. I decided to go to a GI doc to confirm what I had found to be true. She said, “Unfortunately the diet is all you can do.” I mentioned SIBO, and possibly treating it with antibiotics and she was skeptical. It’s very frustrating. I would also add that some psychosocial support should be a part of the team – maybe a support group?
katescarlata
Thanks for your thoughtful comments, Beth. Yes, a support team would be great too! I agree, we do have a long way to go–so we all need to speak up, advocate for ourselves and others and help create changes in the health care system to make the process a whole lot better for those with IBS!!
Ogeal Webster
You are right. We have a long way to go in the U.S.
katescarlata
Ogeal…Yes. We do have a long way to go. BUT the bar is moving. We all need to speak up and be part of the solution.
Kim
I’m not sure if anyone else ever makes this complaint, but I have a pretty generous, all encompassing health insurance plan, but it doesn’t cover a dietitian, even with a referral from a gastroenterologist! 🙁 I realize this is probably a bigger problem within the health care industry, but just some food (ha!) for thought.
katescarlata
Agreed, Kim! Another area where dietitians need to prove their worth to the insurance companies. I am sure dietitian save $$ overall for the insurance plan–by helping the patient manage symptoms.
Wendy A mother of a teenage FODMAP sufferer
I too had this experience with a twist. After my daughter found the FODMAP program and successfully completed the elimination diet, I wanted to meet with a dietitian to make sure she wasn’t missing any essential food group. After a lot of hoops with the insurance company they agreed. But the dietitian wasn’t very helpful. She said that the FODMAP program wasn’t recognized by their association. Then she handed me some printouts from the Internet, which we already had. It’s one of the reasons I’m so glad to have found this blog.
katescarlata
Glad you found my blog, Wendy! Yikes..
Wendy Larson
Kate, What do you think of the Specific Carbohydrate Diet as published over 21 years in Elaine Gottshalk’s Breaking the Vicious Cycle: Intestinal Health Through Diet?
Wendy
katescarlata
Hi Wendy, Anecdotally the SCD seems to show some success particularly in those with IBD–inflammatory bowel disease, HOWEVER, I would love to see more research done on this dietary approach…there is little evidence (research based) to support its use. I think that it is a bit too restrictive overall. I have had a few clients come to my practice malnourished from trying to follow the SCD. My thought is that any diet that restricts fermentable carbs will likely reduce symptoms in those with altered gut microbes and symptoms of hyper-fermentation as seen in IBS. Some microbes are very efficient at breaking down carbs (some microbes have their own carbohydrate metabolizing enzymes). I don’t think there is one set diet approach for all—and that in time w/ more research we will be able to tailor diets more specifically related to our gut microbes. Any diet that modifies carbs in some degree–will likely reduced gas and bloating—often the most bothersome symptoms for patients. Whether you choose to reduce fermentable carbs via SCD (highly restrictive) or low FODMAP (less restrictive)…you may end up with the same symptom management. I personally prefer to make the diet less restrictive initially and modify more if the patient needs it. And lastly, sometimes the symptoms a patient experience are not related to the diet! And other treatable conditions must be explored.