Hello Friends. I hope you had a wonderful weekend and that your week is off to a great start! I enjoyed a wonderful weekend at our little Maine cottage. The weather was picture perfect!
Maine is a special place–especially in the summertime.
Today I thought I would talk a bit about carbohydrates {sound fun?!?} and how FODMAPs fit in the spectrum of carbohydrates.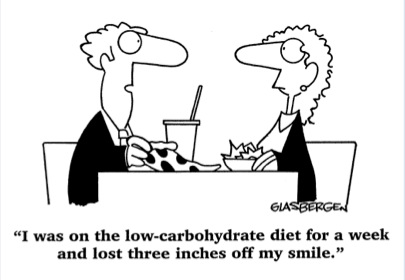
Ha! Ha!
The low FODMAP diet is not a low carbohydrate diet but rather a diet modified in a group of small chain carbohydrates that are commonly malabsorbed by the human body. FODMAPs are rapidly fermented by gut bacteria and pull water into the intestine, stretching the intestine and causing pain, bloating, diarrhea and/or constipation in those with a sensitive gut.
Carbohydrates, for most of us, make up the majority of our calorie intake or about 40-75% of energy needs. I do believe that carb needs varies person to person depending on activity level, weight management needs, genetics and personal tolerance to them.
Carbohydrate digestion begins in the mouth. Starch degrading enzymes are found in the saliva (salivary amylase) and help the body begin the digestive process. Take home message: Chew well and chew slowly.
Carbohydrates are either absorbed in the small intestine or escape digestion when the human body lacks enzymes to break them into digestible components. Digestible carbohydrates are those that are hydrolyzed by enzymes released in the GI tract. Carbohydrates that escape digestion in the small intestine are often but not always fermented by gut microbes. Various gut microbes harbor their own carb digesting enzymes and have the ability to break apart undigested carbohydrates and ferment them in the large intestine…creating gas! Got gas? Well, that is the result of microbes fast at work breaking down carbs your body did not digest! Can’t wait to learn more? Here is a scientific paper on how carb digestion is impacted by our gut microbes.
Carbohydrates are often classified by their degree of polymerization (DP)–the number of sugar units that are linked together.
Monosaccharides: 1 chain sugars : Glucose and Fructose
Disaccharides: 2 chain sugars (DP2): Lactose and Sucrose
Oligosaccharides: 3-9 chains sugars: Raffinose, Starchyose, FOS/ small chain inulin
Sugar alcohols: Sorbitol, Mannitol, Xylitol, Lactitol, Maltitol
Polysaccharides: >10 but often many more! Polysaccharides can be comprised of cellulose, hemicelluloses, pectins, b -glucans, fructans, gums, mucilages, algal polysaccharides & resistant starch. Carbohydrates vary in fermentability. Cellulose, sterculia, and methylcellulose are long chain fibers and are not fermented while water-soluble long chain carbohydrates: resistant starch, pectin, guar gum, and inulin are highly fermentable. Although pectin, guar gum, resistant starch and longer chain inulins are NOT classified as FODMAPs (remember FODMAPs are small chain carbs!}–they are rapidly fermented, and as such, may contribute to gas and GI symptoms in those with IBS. More research is needed in this area.
One of my favorite scientific papers on fiber and functional gut disorders can be assessed here. This is a great scientific review of dietary fiber and fermentation.
As many of your know already, FODMAPs are water-soluble short chain carbs that commonly escape digestion. The ability to digest lactose diminishes with age as the production of the enzyme lactase lessens. Genetics also plays a role. For instance, Asians and African Americans are more likely to exhibit lactose malabsorption than Caucasians.
Fructose, when in excess of glucose in a food is also poorly absorbed for up to 1 in 3 people. Fructose does not require an enzyme to be digested but glucose does aid its absorption. Fructans and GOS are fibers; human lack digestive enzymes to aid their absorption. And sugar alcohols are absorbed via pores in the small intestine. The larger size of sugar alcohols compared to the small pore size in the intestine lends itself to poor absorption.
So, in review, there are many types of carbohydrates in the diet: small well absorbed carbs such as glucose (1 chain carb), sucrose (2 chain carb) and most starches (multiple chain carbs). These are well tolerated by most people. Commonly malabsorbed carbs such as small chain FODMAPs and some poorly absorbed polysaccharides such as resistant starch, pectins and gums can be fermented rapidly resulting in gas production. Research has shown that a low FODMAP diet can help with reduce IBS symptoms. More research is needed to fully evaluate the impact of gums, pectins and resistant starch in individuals with IBS. Because gut bacteria favor carbs for their nutrition, altering carb intake can impact our gut bacteria. Gut bacteria do cause gas, but they also help produce vitamins, help keep our immune system strong, and aid digestion.
The low FODMAP diet has been shown to reduce some gut microbes that produce butyrate, a short chain fatty acid linked with reducing colon cancer risk. The role of diet and our gut microbiome is in the early stages and there is much more to learn. But, due to the potential negative long-term impact on gut bacteria, the low FODMAP diet is recommended to be followed for 2-6 weeks in the full elimination phase. Following up with the re-challenge phase of the low FODMAP diet is important to allow for eating a more varied and nutritious diet as possible without triggering symptoms.
And I know some of you really struggle with carbohydrates in general. I do think that carbohydrate tolerance can be very variable depending on the microbes that inhabit our gut, the degree of inflammation occurring in the small intestine (whether from microbes, inflammatory bowel disease, untreated celiac disease, autoimmune conditions and SIBO) to name a few potential causes. Work with a gastroenterologist and registered dietitian well-versed in digestive health to help properly evaluate the function of your GI tract and guide you on eating most varied and nutritious diet possible.

Margaret VanDyke
I had the breath test yesterday and have no feedback yet from the doctor but the indicator reached 4. I do know that I started belching about an hour after ingesting the stuff they gave me to drink and that it caused me to have diarhea later in the afternoon and this morning. Kate, I am desperate. Is that enough proof for the dr.to give me rifaxim? Oh, I know you can’t answer that, but would you in your MUCH greater knowledge about this, think that I have SIBO? I have been suffering with the belching, bloating and gas for months..actually years. I am desperate.
shel miller
Hi Kate:
Keep enjoying Maine!
I wanted to read that paper you mention:
papers on fiber and functional gut disorders can be assessed here
but the link brought up a blank at the website, nature.
katescarlata
That’s weird–because when I click it–it brings the article up. Sign up for Medscape—it’s free and try this link: http://www.medscape.com/viewarticle/804450 Or try again with Nature at this link: http://www.nature.com/ajg/journal/v108/n5/full/ajg201363a.html
Sally Crusan
I’m new to this site. Trying to “digest” all the great info. I live in Wells, ME year-round That’s the most palatable part of my day lately!!
katescarlata
Lucky you, Sally! I am loving Maine!! Glad you stopped by my blog!
sandra
I have been on my lowFODMAPs diet for 3 years now. Seeing a practitioner and have done work on bacteria and gut healing but am still stuck with problems with my original offending foods. Any ideas or am I stuck on these restrictions forever??
katescarlata
Sandra, most people can add some FODMAPs back into the diet. If you have no wiggle room adding foods back, I would work with your dietitian and GI doctor to explore overlapping reasons/causes for your food intolerance.
Cameron
Hello. I have SIBO, and I have a question about toothpaste. My toothpaste contains sorbitol (which if I’m not mistaken, is a FODMAP). I have been on a low FODMAP diet, and have been trying to avoid FODMAPs. My question is, is it possible for the sorbitol in my toothpaste to exacerbate my SIBO issues? (or is it fine as long as I don’t swallow the toothpaste?) Thank you.
katescarlata
Cameron, the sorbitol in toothpaste should not pose a problem since you are not eating it!