This Mast Cell Activation Syndrome (MCAS) post (part 2) will include information via two patient’s perspectives along with the potential role of supplements, pharmaceutical treatments and online resources.
I was very happy to see in my literature search that this is a growing area of research with more and more papers on mast cell activation disorders! With that being said, there remains much more work to do to understand the complexities associated with managing the spectrum of mast cell disorders.
Please note, this is not a comprehensive post on mast cell activation syndrome. The purpose of this post is to introduce the topic, along with the patient’s perspective and a brief sampling of the research in this area.
Additionally…do NOT self-diagnose…work with your PCP and an allergist/immunologist to guide you in a proper, individualized diagnosis and treatment.
For an introduction on this topic, see my Mast Cell Activation Syndrome (part one) post here.
Some science basics for this post:
Too much histamine in the body can lead to histamine intoxication such as can occur after eating spoiled fish, a condition called Scombroid poisoning. Scombroid fish poisoning, or histamine fish poisoning, resembles an allergic reaction that occurs after eating fish contaminated with high levels of histamine.
What does this have to do with mast cell activation syndrome?
Mast cells house histamine in the body. One of the key ways of treating mast cell activation is to stabilize the mast cells so they do not release inflammatory chemicals such as histamine (and other inflammatory chemicals) OR to block the effects of histamine via anti-histamine medications.
The amino acid, histidine, can be metabolized into histamine via our gut microbes. The body metabolizes histamine in two known pathways via HNMT (histamine-N-methyltransferase) or via degradation by diamine oxidase (DAO), which helps rid the body of excess histamine.
We will discuss the role of a low histamine diet for mast cell activation syndrome, in the 3rd series post on this topic. Spoiler alert: there is little scientific data on this topic.
Medications commonly used for mast cell activation syndrome include H1 blockers, which suppress histamine mediated effects; H2 blockers, which block the action of histamine at the histamine H2 receptors of the parietal cells in the stomach and mast cell stabilizers.
More specifics on medications used in mast cell activation later in the post.
The Patient Experience
I interviewed 2 clients who have been diagnosed with mast cell activation disorders. I will refrain from using their names for privacy issues, but will instead provide info via Client #1 and Client #2.
Interestingly, but not surprisingly, both clients mentioned how thankful and relieved they felt to ‘finally’ reach a diagnosis. Receiving a diagnosis, alone, was a stress relief and helped with their healing process.
First, let’s talk a bit about their presenting symptoms and experience:
Client #1 primary symptom profile included: gastrointestinal symptoms, back pain, chronic bladder pain, “off the charts” anxiety that culminated with the additional symptoms of itching and angio-edema (rapid swelling beneath the skin or mucosa).
“My body was completely swollen. I have found stress and my diet to be my biggest triggers. To lower stress, yoga has been helpful along with finally, having a diagnosis. I had a couple doctors tell me I was crazy. It took about 1 1/2 years to finally get my symptoms fully under control. If you think of your body as a ‘bucket’ and it is full of inflammation, it takes a while to empty the bucket. For me, my mast cell issue hit a critical mass and I felt like I was on a run-a-way train.”
“After treatment, and finally a diagnosis, I feel so much better. I look at food as medicine. I don’t focus on the foods I have removed from my diet but rather focus on what I am gaining healthwise by removing the food triggers.” (More on nutrition and mast cell in the next post!)
Client #2
“It took me about 5 years to get a diagnosis. I had been seen by specialists at Massachusetts General Hospital, Beth Israel Deaconess Medical Center, and New England Baptist Hospital. I had a bone marrow biopsy because they thought I had leukemia.”
Finally getting a diagnosis was so helpful. “You get frustrated being misunderstood. You start to doubt yourself. My primary symptoms included, brain fog, facial flushing, sore throat, lip and tongue swelling, allergies, weight loss. I found I bled more easily too.” (Heparin can be released from mast cells, thinning blood & contribute to easy bruising).
Additional symptom triggers for Client #2 included odors from cleaning products, flowers, and the environment.
A bit of advice to you from Client #2, “Report all reactions you have to your doctors. I had a terrible reaction to an IV contrast given during a test that I did not report, that may have led to an earlier diagnosis.”
IV contrast can lead to mast cell activation; share this reaction to your doctor.
Medications and Supplements
Of course, do not self-medicate. Discuss medications and supplement use with your healthcare provider prior to use.
Here is a nice outline of pharmaceutical treatments that many be used outlined beautifully by The Mastocytosis Society.
H1 blockers –may include names like Zyrtec, Claritin, Xyzal
H2 blockers –may include names like Zantac, Tagamet, Pepcid
Leukitriene inhibitor (Leukotrienes are believed to play a major role in causing the symptoms of hay fever and asthma.)– Singulair (learn more here).
Cromolyn-mast cell stabilizer
Ketotifen-mast cell stabilizer and blocks H1 receptors on mast cells.
Check out this article to learn more about pharmaceutical treatments for mast cell disorders.
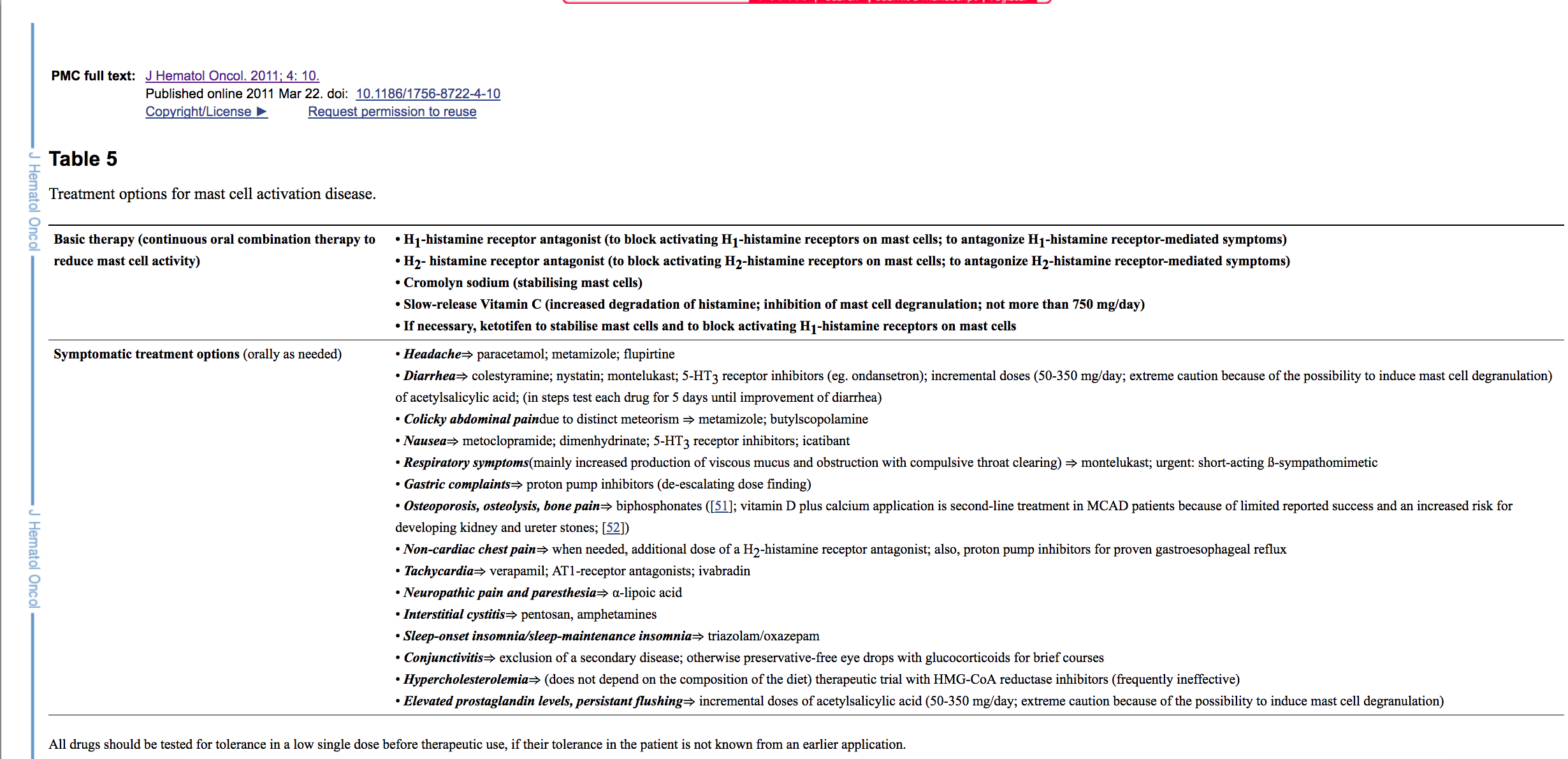
Another review of mast cell activation and treatment therapies can be found here, and see below, note the medications detailed in Table 5.
Supplements
There are many deficits in the medical literature in this area. Supplements are poorly regulated making this area a little murky too. This does not mean they are not helpful for some but rather there is much more to learn.
Client #1 has tried supplements and is unsure if they are helping but since she feels better has remained taking them, including Neuroprotek from Theo Theoharides, MD, PhD.
Client #2 has put her focus on expanding her diet as a way of healing her body. She has found salicylates in food and supplements to be a trigger for her, so avoids foods and supplements that may contain them. She does use magnesium supplements to keep her bowel movements more regular.
From what I have read, the use of supplements as well as nutritional treatments needs to be individualized and we truly need more research! Some supplements work better for some than others. Genetic makeup, such as having the MTHFR gene defect (learn more about this genetic defect here), may additionally impact what supplements are tolerated.
Speaking of genetics, there are genetic SNPs, also pronounced as “snips” (single nucleotide polymorphisms, the most common type of genetic variation among people) associated with lower DAO activity, (remember DAO helps the body degrade and remove histamine). Diamine oxidase serum activity was significantly associated with seven SNPs within the DAO gene. DAO gene variants strongly influence DAO expression and activity. Article here.
DAO supplements
There is limited research to support the use of DAO supplements and no access to a validated test in the US to assess DAO activity (as far as I know!)
My colleague Wendy Busse, has a great review on DAO, find it here.
Quercetin
More human studies are needed, however, quercetin in test tube and animal studies reveal that it can prevent mast cells from releasing histamine. It also functions as a antioxidant and anti-inflammation agent in the body.
Vitamin C
More research is needed to determine dosing and relationship to mast cell activation syndrome, but Vitamin C does appear to reduce symptoms of diseases associated with mast cell activation. There is some caution in using high doses of Vitamin C due to increase risk of calcium oxalate stones, blood in the stool, and diarrhea. See this interesting science paper about the relationship between Vitamin C, Mast Cells and Inflammation.
Online resources for wide range of mast cell disorders:
A few words of wisdom from clients living with mast cell activation disorders to you:
- Celebrate every success, no matter how big or small.
- You will find out who your true friends are as well as what it means to be a true friend in times of challenging health conditions.
- Do your best to manage your symptoms and adjust to your “new” normal life.
- Find new hobbies or activities if your old hobbies/activities contribute to symptoms. (one client stopped playing tennis but instead works out at her own home with a personal trainer).
- Since mast cells may bother your eyes, try audible books and give your eyes a rest.
- Remember worry and stress makes symptoms worse, incorporate new ways to manage stress (yoga, maybe?)
A big thank you to my clients for sharing some of their journey for this post! xx
That’s all for today, friends. I have to say this area of science is very interesting but very complex.
My next post, I will talk about diet and stress. Stay tuned.

Eileen
Thanks for this. What is the connection with Leaky Gut and this? Is there concern that taking H1 or H2 blockers could lead to Leaky Gut?
Kathy
These articles have been very helpful & informative! When can we expect part 3?
Have you had patients with MCAS require enteral feeds?
katescarlata
Thanks Kathy! I hope to post the third post soon. I have not seen anyone require enteral feeds for MCAS in my practice, anyway.