Hello Friends. Today’s topic is a quick review of some of the research that was presented at Digestive Disease Week (DDW), the BIG US based GI conference on May 21-May 24, 2016.
I spend a few days running (seriously! I put in over 14,000 steps/day) around the San Diego convention center to attend meetings on gut health. It is an exciting time in this area of research, especially as a registered dietitian, as more and more studies are pointing to the role of nutrition/diet and changes in its impact on the gut microbiome. Changes in our gut microbiome can make the difference between health and disease.
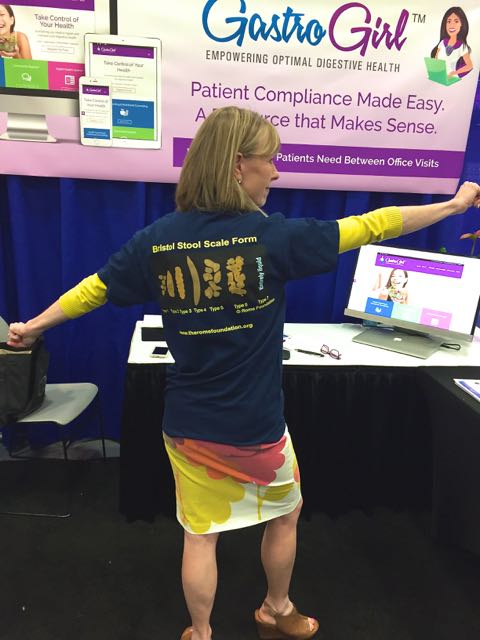
We like to have fun at DDW too! Here I am with my Bristol Stool Chart at the Gastro Girl booth, a new novel telehealth and online community that I have been working with for people that suffer with GI conditions!
I would like to share with you a few interesting topics covered during DDW:
Food Additives and Inflammation:
The intestine is protected from gut microbes that inhabit our intestine via multiple layers of mucus structures that cover the intestinal surface. The mucus layer in essence is a safety layer, keeping microbes from invading the inner lining of epithelial cells of the intestine. Emulsifiers have been implicated in disrupting the mucus layer.
Food emulsifiers are detergent like compounds that are added to a wide variety of processed foods–and are approved as safe and may be lurking in your carefully selected and yes, even in organic foods. But more research is linking polysorbate 80 (P-80) and carboxymethylcellulose (CMC) to changes in the gut microbiota, increasing likelihood of inflammation, intestinal permeability (leaky gut), and a reduction of mucus in the intestine. Hirotaka Furuhashi of Japan presented a paper at DDW on P-80 and carboxymethylcellulose- using small intestines with lesions from just-killed mice to demonstrate that the common food additive P-80, increased the injured area promoting damage of the small intestine.
A group of researchers from the US at Georgia State: Benoit Chassaing, Tom Van de Wiele and Andrew Gewirtz group had previously demonstrated in their research that dietary emulsifiers (P-80 and CMC) results in alterations in the gut microbiome (increase in bioactive LPS and flagellin–bacterial components linked with inflammation)–these changes are linked with metabolic syndrome and colitis. Intake of both P-80 and CMC increased potential pro-inflammatory effects. P-80 alters the composition of the microbiota, favoring species that express more flagellin, while CMC,increases motility genes. More on this topic here.
Could the wide use of food emulsifiers be a contributor to the rise of inflammatory bowel disease? Perhaps. And this is just one reason, that I encourage that the majority of your food choices be from whole foods vs. products.
SIBO and Carbohydrate Malabsorption Topics
One of the most frustrating issues for me in the treatment of SIBO has been a lack of standardization for diagnostic measures of SIBO as well lack of research on dietary interventions for people that suffer with this condition. SIBO is a condition in which an abundance of microbes invade the small intestine. Typically, the small bowel should not house that many resident microbes.
At DDW, Ali Rezaie, MD from Cedars Sinai presented Hydrogen and Methane Based Breath Tests in GI disorders: Report of the North American Consensus Meeting. A small group of physicians from the US, Mexico, and Canada met to strategize and attempt to provides some standardization for breath testing for SIBO and carbohydrate malabsorption. Some general agreements regarding testing and results of breath testing were presented at DDW:
- For both glucose and lactulose, SIBO breath tests with a rise greater or equal to 20 parts per million of hydrogen by 90 minutes was deemed a positive test result and a result of greater or equal to 10 parts per million of methane anytime during the test was deemed positive.
- SIBO should be excluded prior to undergoing breath tests for carbohydrate malabsorption (fructose and lactose test). This is key as a lactose or fructose test may be positive in the setting of SIBO. (The bacteria in the small intestine consume the sugars before than can be absorbed!) When the SIBO is treated, the fructose and lactose malabsorption may no longer present.
- Two peaks in a breath test are NOT required for the diagnosis of SIBO.
- Fructose and lactose breath tests should be performed for at least 3 hours.
- A rise greater or equal to 20 parts per million for lactose or fructose breath tests=positive test.
Satish Rao’s group from Augusta, Georgia presented a study looking at small bowel transit and found that those with SIBO has a delay in small bowel movement. Treating the movement by use of prokinetic medications such as low dose erythromycin appears to be one treatment modality to address this issue.
Another study presented at the conference on breath tests for SIBO, revealed that about 1/3 of 1,000 subjects studies with persistent GI symptoms had a positive breath test for SIBO or carbohydrate intolerance. Should most patients with IBS be tested for SIBO? This remains an unanswered question. If you asked me, I would say, if the patient experiences bloating or post meal fullness, absolutely, YES!
Brain Fog and Alterations of Intestinal Microbes
Satish Rao’s group also reported on the relationship of microbial end products including d-lactic acid that may play a role in brain fog in a subset of patients with dysbiosis. A paper back in 2009 reported a connection between chronic fatigue and d-lactic acid production, click here. D. lactic acidosis may present as: headaches, weakness, cognitive impairment, fatigue, pain and severe lethargy.
FODMAP updates
Well, good news here…University of Michigan’s Shanti Eswaran, MD presented here research findings from a randomized, controlled trial comparing a low FODMAP diet to a standard IBS diet (NICE guidelines). Patients on the low FODMAP diet showed greater improvements in quality of life indicators after 4 weeks compared to the other IBS diet therapy. More than half of the study participants experienced a symptom response to the low FODMAP diet with robust improvements in pain and bloating. Dr. Eswaran’s group also noted health related quality of life improvements on those following a low FODMAP diet including better sleep quality and improvement in anxiety levels.
Shi-Yi Zhou, also at University of Michigan reported on his interesting study evaluating the impact of the low FODMAP diet and visceral hypersensitivity. This study reveals a change in lipopolysaccharide (LPS), the outer layer of the cell wall of gram negative bacteria and is also an endotoxin. LPS is associated with inflammation, diabetes and obesity. In Dr. Zhou’s study, he found that patients with IBS-D had elevated levels of LPS which induced visceral hypersensitivity (a greater sensation of pain) and impairment of the mucus layer in the intestine. The low FODMAP diet normalized LPS levels and restores the mucosal layer and reduced the sensitivity of the intestine, collectively leading to symptom improvement.
I was also happy to see topics around bile acid diarrhea (BAD)–as I feel this is a problem for some of my clients with IBS-D. I did a post about BAD a while back, check it out here.
There was also some dialogue about evaluating digestive enzyme levels via intestinal biopsy. I have been asking for this to be done for YEARS!! The testing requires dry ice….and to be shipped to a lab that can test for the presence of digestive enzymes. NOT rocket science! These tests are often checked in children, but not in the adult population. I do believe in the setting of inflammation in the small intestine, there may be a reduction in digestive enzyme production. Hopefully, testing will become more routine in a subset of the adults who’s symptoms are suggestive of carbohydrate malabsorption!
Of course, this is just a snap shot of what I learned over the conference! DDW is a great conference to learn from some of the best researchers in the world. Maybe I will see you there next year in Chicago?

Rebecca
Thank you for this post. It’s good to know that more research is being done for digestive issues.
Susan
Brilliant! Thank you so much for keeping us in-the-loop as new findings are presented. It’s so encouraging to know that progress is being made and that gut problems are being taken seriously. Sometimes one can feel isolated and a little freakish, and your hard work shines a light on our conditions!
Susan
Brilliant! Thank you so much for keeping us in-the-loop as new findings are presented. It’s so encouraging to know that progress is being made and that gut problems are being taken seriously. Sometimes one can feel isolated and a little freakish, and your hard work shines a light on our conditions!
katescarlata
Glad you liked the post, Susan! I appreciate your comment! 🙂
Jane Harris
This is great news. I am so impressed at the University of Michigan website about the Low FODMAP diet! Yay U. of M.! I have been recommending it to all my friends…so easy to understand/user friendly. Apparently nobody in the Chicago area has ever heard of this diet (at least in my experience)(:
katescarlata
They have heard of FODMAPs in Chicago 🙂 Try U of Chicago! The low FODMAP diet is gaining traction—it will be a household name before long!
Linda M.
Kate,
Here is another issue too. My doctor had me complete a Hydrogen Breath Test; but he did not tell me to have certain type of diet before the testing, or fasting. Next week I will be treated for Sibo, but I don’t know if I really have it; symptom of Sibo are pretty much what I am experiencing. In addition, I see where the antibiotic should be 3 a day, but he only prescribed two a day. So, I am in the position of either telling him all the Sibo sites say you need three a day. This is extra stress that I do not need. I feel very helpless right now.
katescarlata
Absolutely speak up to your doctor and discuss your concerns. Many doctors are not well versed in SIBO management –so you need to speak up and share what you have learned.
dancinA
Thank you for the updates. They’re always very helpful. I actually see Dr. Rezaie in Los Angeles, and I’ve had some of the breath tests, but not all. Was there any mention at the conference of the IBScheck blood test that checks for antibodies to Vinculin which indicates post infectious IBS? I tested positive on that one. I want to add that I have tried so many approaches for my IBS-D but nothing has worked long term. I am now on my third round of Rifaximin, as well as taking Zofran, which causes other issues. I didnt see much difference with the initial FODMAP diet but as you’ve said, it needs a trained dietician, and unfortunately, this is not covered by Medicare or any insurance, so it’s hard to follow it long term.
katescarlata
Many insurances cover nutrition services–it varies state to state. Yes, the talk did mention IBScheck–but this was not new information–as I have discussed this topic already on my blog.
dancinA
Thank you, Kate. I have yet to find a dietician that knows about FODMAP and is covered by insurance. Even the one at the UCLA GI office is not covered because they have separated the dietitians that advise about weight loss and diabetes (covered) from the one who knows about FODMAP (not covered). Very frustrating.
Carrie Glicksteen
Thank you so much for this report. I
dkaj
Kate, thanks once again for keeping us all updated on everything GI related. I have to say I Love your new Gastro Girl Name and Logo. IT Rocks!!! You should team up with an Elasti Girl from the EDS hypermobility community to help shed light on how the weak connective tissue and collagen can affect the GI tract and how their GI symptoms can be compounded by fodmaps. If I had to pick someone, I think Crystal Saltrelli would be your perfect candidate.