Banish your bloat with the low FODMAP diet. The low FODMAP diet is a dietary approach used to minimize symptoms of irritable bowel syndrome (IBS). This diet is effective in managing symptoms for 3 out of 4 individuals with IBS and was designed by Australian researchers at Monash University. I was fortunate to visit the Monash Team in September 2011 and continue to keep in touch and will be collaborating on an upcoming study on food analysis.
Click here for my FODMAPs 101 handout. This handout is a 2 page handout that introduces the low FODMAP diet. Dietitians: This handout can be used with patients as you introduce them to the low FODMAP diet concept.
FODMAP is a acronym…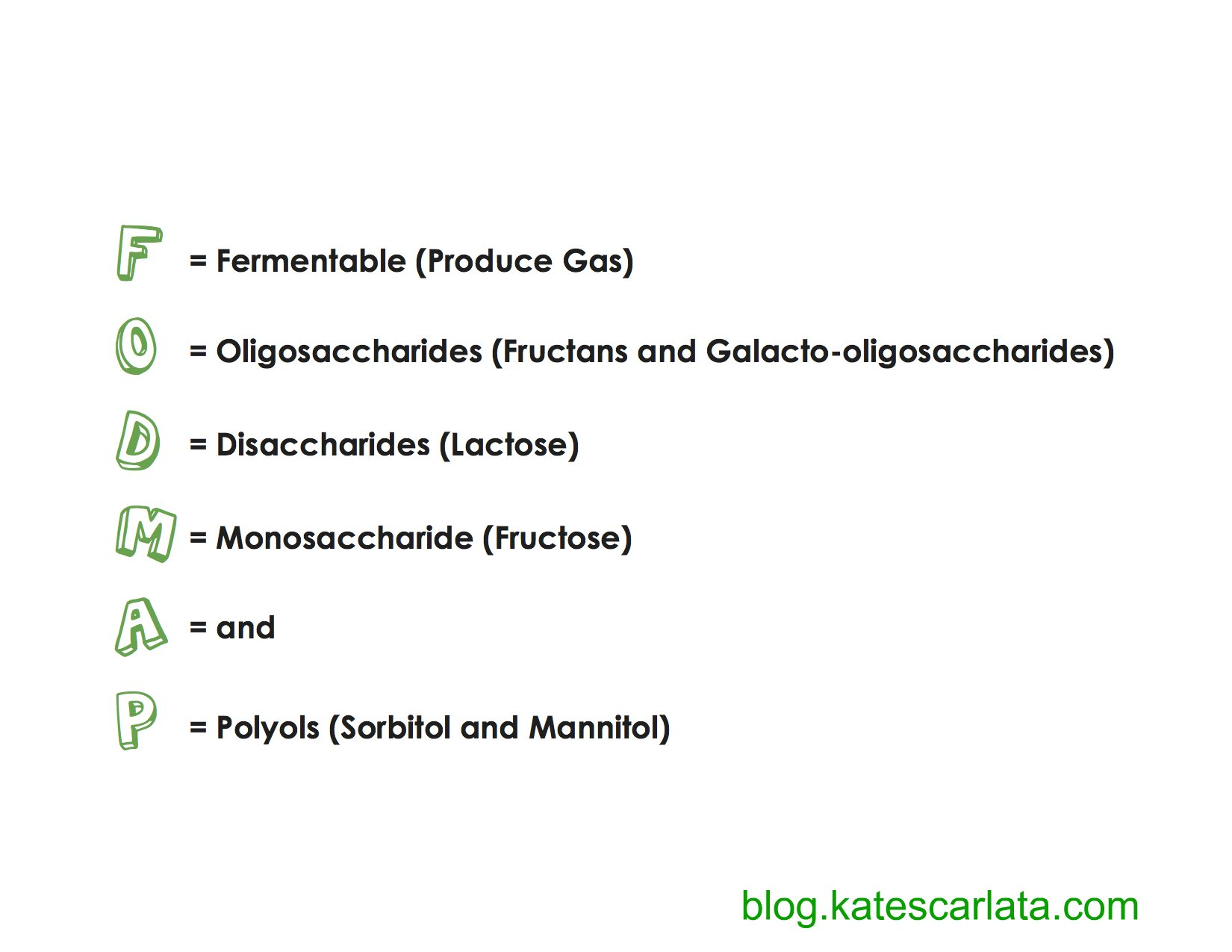 So in short, the F in FODMAPs stands for fermentable or ‘creating gas’, the O stands for Oligosaccharides, water-soluble fibers which are found in wheat, onion, barley, rye and garlic. And please don’t forget chicory root extract (inulin) added to so many foods to boost fiber! The D stands for Disaccharides which is lactose found in milk, yogurt and ice cream. The M stands for monosaccharide or the sugar, fructose, when present in foods in excess of the glucose content–found in some apples, pears, watermelon, honey and agave syrup! And P is for polyols A.K.A sugar alcohols found in peaches, plums, apples, cauliflower and mushrooms and added as artificial sweeteners in sugar free gum, mints and some medications.
So in short, the F in FODMAPs stands for fermentable or ‘creating gas’, the O stands for Oligosaccharides, water-soluble fibers which are found in wheat, onion, barley, rye and garlic. And please don’t forget chicory root extract (inulin) added to so many foods to boost fiber! The D stands for Disaccharides which is lactose found in milk, yogurt and ice cream. The M stands for monosaccharide or the sugar, fructose, when present in foods in excess of the glucose content–found in some apples, pears, watermelon, honey and agave syrup! And P is for polyols A.K.A sugar alcohols found in peaches, plums, apples, cauliflower and mushrooms and added as artificial sweeteners in sugar free gum, mints and some medications.
Everything you need to know about FODMAPs or just about can be found in this section.
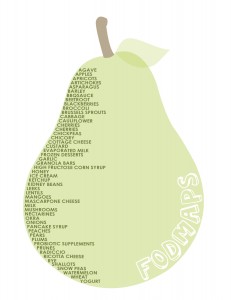
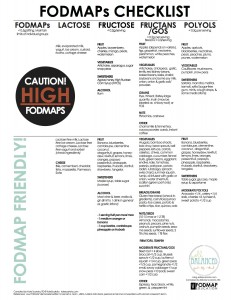
This section provides all sorts of references for you to use while you are beginning your journey on the low FODMAP diet. Items such as the FODMAPs check list
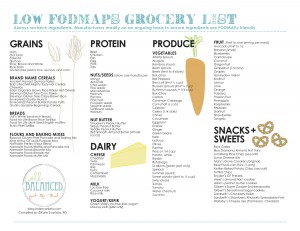
And my very handy low FODMAP shopping list.
Looking for some menu and snack ideas, check out this handout!
But there are SO many other helpful resources in this section for dietitians or individuals that want to learn more about the low FODMAP diet. Just hover over the FODMAP Basics tab to find great information that will help you navigate the low FODMAP diet. But most importantly, please work with a dietitian knowledgeable in the low FODMAP diet to ensure you are following it correctly and meeting your nutritional needs.
Oh, yeah..if you are looking for RECIPES…check out my recipe section here! Or visit my Pinterest page for more ideas.

Stacy Campbell
Hi Kate…why are probiotic supplements on the list above as being a fodmap. I take 2 day…they are both gluten and lactose-free. Should I not be taking them? I’ve never seen them on a list before…I am new to fodmap. Thanks.
katescarlata
Stacy–
Probiotic supplements WITH chicory root or inulin would be a potential issue not probiotics in general. Hope that helps.
Sweden
Avocado, is it okey to eat and how much? What kind of bread is possible to make?
katescarlata
Just about 1/8 of an avocado at a sitting is okay. Gluten free bread is best made without FODMAP containing ingredients.
Ann mcgrath
Spelt bread is good. Just spelt flour, yeast, a little sugar and salt + water.
Mary Drake
Should I take a probiotic with inulin? Should I drink cider vinegar? I’ve been on love fodmap for weeks.
katescarlata
Hi Mary, I would suggest you ask your dietitian–and if you are not working with one–I would recommend you do!
megan
What is invert sugar? Is it considered a FODMAP offender?
katescarlata
Invert sugar is low FODMAP in small serving. It is simply table sugar that has been broken apart in equal amount to glucose and fructose. When fructose is in excess of glucose it tends to be more of an issue….but Too much table sugar at one sitting–contributes to potentially too much of a fructose load– so limiting sweet treats to 1 serving including fruit to avoid too much fructose at once is a good idea. I hope that is not too much rambling for you!!
megan mullin
Thanks Kate, So foods from the fruit group and sweeteners that are “safe” should be limited to 1 serving per meal or sitting? What about veggies in the fodmap friendly group?
katescarlata
Fruits should be limited to one serving per sitting or meal OR spaced out at least 2-3 hours. Veggies are less of a problem unless in the ‘fructose’ group (per my check list)–that is my understanding anyway…
Kim
I was wondering about black eyed peas and purple hull peas? Are they ok to eat? I have been following the FODMAP for about a month but we have a freezer full from our garden and was wondering if they were ok to eat?
katescarlata
Not sure Kim if they have been tested for FODMAP content–but if I had to guess, I would surmise they are not low in FODMAPs–probably source of fructans and GOS.
Jolante
Hi Kate
I have been doing the low fodmaps diet for some time and it works fantastic! Thank you for all the info! I was wondering about celery seeds were they fell. I have heard many great things about them and the nutritional benifits they give the body so I was curious if you knew about them?
Thank in advance
Samantha
is soy lecithin a low fodmap food?
katescarlata
Samantha, Yes soy lecithin should not be an issue on the low FODMAP diet to the best of my knowledge.
Samantha
thats good. I want to make my own yogurt as its cheaper than buying the expensive low lactose probiotic yogurts and the packet stuff is gluten free too and still doesn’t have additives and gelatin and all the other crap yogurt seems to have added to it! but it did have soy lecithin in with the milk powder so I had to wonder…..I try to avoid soy when I can but sometimes its just not possible when your making sacrifices everywhere else! another quick question, what about pineapple? is that a low fodmap food? I’ve seen on some lists, it is and then it isn’t????? I have ordered the booklet from monash and still waiting for it to arrive but in mean time I’m still having to live and eat lol…..
katescarlata
Pineapple is low FODMAP–Monash lists the portion to be 1/2 cup. Feel free to ask questions while you get ramped up and are in the learning phase. I think small amounts of Greek yogurt is a nice option for many too….if you limit the portion—Chobani has about 4-5 grams of lactose in the plain yogurt per 6 ounces and many people can tolerate up to 4 grams per sitting. So maybe just eat about 4 ounces and test your tolerance…
Lauren
Hi Kate,
I’ve read on some websties that pineapple has fructans. Is that not true? Or is it just trace amounts?
Thanks!
Lauren
katescarlata
Lauren–there are lots of out-dated lists online. The Monash team has pineapple as low fructan.
Samantha
oh good! love pineapple! I only have a small amount of yogurt with my breakfast but its still a good source of morning protein, calcium needs and those wonderful probiotics that help our tummies too!
Katie
Thanks for your reply Kate.
The vitamin C ingredients are:
glucose, saccahrin sodium and…WAIT! wheat derived maltodextrin.
Could that do it?!
It may have also been almond milk that was upsetting me.
Also – have you heard of people having problems with soy protein? I’m finding it hard to tolerate fructose friendly muesli and I think it might be the milk I’m having it with – I’ve tried both protein and bean derived soy and they both cause bloating. Either that, or the muesli isn’t as fructose friendly as it states. I noted that it does have quite a lot of almonds in it.
I also had a couple of strawberries today that upset my stomach but I think they were overripe.
Kate
katescarlata
The maltodextrin by definition should not pose a problem. Some parts of wheat are not FODMAPs. Maltodextrin and wheat starch are two examples of non-FODMAP wheat ingredients.
I wonder if it is the muesli–the combo of oats and almonds is likely too much of a FODMAP load as they both contain moderate amount of FODMAPs–GOS and fructans–so the combo could be over your threshold.
Soy tolerance is variable==try minimizing it and see if you notice a difference.
Morgan
Hi Kate- I am having trouble finding a Calcium plus D and multivitamin that is Fodmap safe. Do you have any brands you could suggest?
katescarlata
Try the Vitamin Shoppe with calcium citrate, vitamin d and magnesium.
Dawn Halstead
I was told to avoid magnesium as it triggers diarrhea. Then, I find that most of my medications for reflux have magnesium in them! Is there a “safe” magnesium that I can use? I also need a Vitamin C supplement, but which one is FODMAPS Safe? thank you.
Melodie
OK
I have a list.
I’ve been saving up questions and comments!
First, I love your blog. Thanks so much for making Fodmapping less overwhelming. I’m a fodmap mom. In other words, I’m trying to guide a child through the Fodmap world. It’s not easy!
First a tip for your fans, Betty Crocker now has gluten-free mixes. We tried the chocolate chip cookies and the whole family, and our guests, loved them.
Now for questions:
What about marshmallows and rice krispie treats (which are made with them) for Fodmappers? They don’t have HFCS, but they do have corn syrup. The rice crispies also list fructose, soy bean oil, soy lechithin, and corn syrup solids. But the main ingredient (toasted rice cereal) is OK. How do I know if something is not enough to cause a problem or if it is too much. Marshmallows list corn syrup as a main ingredient.
I know soy is not OK for fodmappers, but what about soy oil and soy lecithin?
Has anyone found a good non-dairy, non-soy creamer for their coffee?
katescarlata
Hey Melodie!
The Betty Crocker GF chocolate chip cookies do look good. No major FODMAPs except we still don’t have definitive on the chocolate chips. But as I have said before they don’t seem to be a big issue for most of my clients.
I like the GF rice krispies that are made with sugar vs. high fructose corn syrup. The marshmallows should be okay. Soy oil and soy lecithin are not a FODMAP source. Also, as an FYI–I love the Shopwell site–you can add in food ingredient you want to avoid and it helps sorts foods for you AND it is easy to plug in a food and find brand names and ingredients listed…a huge time savor for me and a great tool when creating a low FODMAP shopping list!
http://www.shopwell.com
Melodie
Thanks so much!
Jena
Is regular rice krispies cereal ok or does it need to be a gluten free version? I looked at the ingredients and nothing jumped out as fodmap to me. What about crispix? Trying to save money where I can and not have to buy all GF products
katescarlata
The regular rice krispies cereal should be fine. Just be sure it does NOT have high fructose corn syrup. Crispix looks okay to me too–though corn products can vary…but I think it should be okay.
Samantha
Hi again!
I’m getting mixed messages all over the web about coconut milk/cream…..is it fodmap friendly or not??? some say yes its fine others say no its not???!!!
katescarlata
Samantha–Coconut milk is okay. I have not seen any info on coconut cream. OLD data had coconut milk as a source of excess fructose but the app from Monash has it as okay–green light.
Elizabeth
I am having a hard time determining whether “coconut milk” is referring to the carton type near the dairy milk or the canned variety near the Asian cooking section of the grocery store. I love Trader Joe’s light canned coconut milk in place of cream for my tea, smoothies, etc. I believe the canned is the meat and the milk of the coconut. Not sure what the carton stuff is but I do know it contains things like carageenan and guar gum that I try to avoid. The FODMAP lists I come across don’t discriminate which type it is referring to. Thanks in advance!
katescarlata
Hi Elizabeth, I confirmed with 2 of the Monash researchers that the coconut milk that was analyzed was the traditional canned coconut milk not the boxed carton varieties. I love the Trader Joe’s light canned coconut milk for the same reason–free of gums and carrageenan! 🙂
Samantha
Well thats great! Thanks for that!
Rachel
Just found your website, 7 day on the FODMAP. Your blog is so helpful. Thanks from Rachel in Calif.
katescarlata
Glad you stopped by Rachel!!
Samantha
Hi Kate, I’ve just been to see my dietitian and she told me that cooked apple like apple puree found in many gluten free baking recipes is ok on a low fodmaps diet…..is this right??? Apple was a big tummy trigger for me but I always had it in raw form. Am I best still avoiding it even if cooked???
katescarlata
Samantha-NO apple on the low FODMAP elimination phase cooked or raw.
Samantha
Thanks Kate, it was a big trigger for me and don’t really want to touch it again! No apple what so ever then! Do you have a suggestion of what I could use to replace apple puree in gluten free and healthy baking???
katescarlata
How about lactose free yogurt for the apple puree or perhaps mashed banana? Depends on how you are using it.
Samantha
I’ve used mashed banana before and worked great so I’ll go with that!
Nina O'Brien
I have used rhubarb in the same way with success too.
emmie
Hi Kate,
I am sooo glad I came across your website. I feel the information you provide can be trusted and that is so important. Thank you so much!!
I have SIBO due to slow mobility secondary to scleroderma. For me, the end result is constipation. I am on a once a month antibiotic (rotating between 3 antibiotics) to hopefully get rid of the bacterial overgrowth. I use Mirilax to help with the constipation. My doctor also gave me a copy of the FODMAP foods to avoid and those that are friendly. He said to follow it as much as possible, but that I didn’t have to go crazy just follow it as much as possible.
I know from a past elimination that gluten doesn’t bother me. That situation could change from what I understand. Lactose does bother me unless I take Lactaid before eating a food containing milk or milk products. I have continued to use Lactaid in this way while trying to follow the FODMAP food plan. What are your thoughts on this? (Sorry so wordy.)
Thank you very much,
emmie
katescarlata
Hi Emmie,
Glad you stopped by my blog. I have personally suffered with SIBO so I empathize with you. Not fun.
Even if gluten in foods do not trigger gastrointestinal symptoms the fructans (one of the FODMAP sources) in wheat, barley and rye can contribute to IBS symptoms or can become food for gut bacteria so I would not encourage you to go overboard with those ingredients. If you are lactose intolerant, I would try to limit your lactose containing foods and rely on the lactaid pills for special occasions as they may not be completely efficient at breaking down the lactose in foods you eat. When lactose is not completely digested it will become food for bacteria. Certainly an occasional ice cream with a lactaid pill should be fine. FODMAPs are like fast food for bacteria. I don’t think you have to be super strict with the diet but less of these FODMAP rich foods may minimize your risk or potentially increase the time between SIBO reoccurrence.
Pam
Hello, I was wondering how bad the mannitol is in lactaid. I cannot find a lactaid type pill without Mannitol (why they add a sweetener to a pill you swallow I will never understand) which is one of the FODMAPS. should I not test or have any dairy until I have tested Mannitol?
Thanks
katescarlata
Pam, if that was the only mannitol in one or two tabs you might be okay. Or try this one. It has glycerin–but might be okay. http://www.puritan.com/puritans-pride-brand-0102/super-lactase-enzyme-125-mg-004932?scid=37958&cmp=gpl-_-digestivehealth-_-004932&gclid=CLz869zVztACFZZMDQodc78EYQ&noredirect=true&ssl=1
Sara
I’m an RD who is interested in learning more about the FODMAP diet for the purpose of helping my patients. What resources should I use to ensure I have a solid understanding of the diet and how to implement it? Thanks for your help – your website has a lot of good information!
katescarlata
Sara, My blog has lots of great handouts—look under the fodmap basics tab for shopping, check list, menu and snack ideas. Also, I have written a continuing education program with Wolf Rinke which walks you through the diet. The Q and A section allows you to really apply what you learn. http://www.wolfrinke.com/CEFILES/C226CPEcourse.htm
There are some wonderful research articles as well. One of my favorites is out by Sue Shepherd and Peter Gibson. Here is the abstract but you should be able to get on line. http://www.ncbi.nlm.nih.gov/pubmed/22488077
Melodie
Do we know if some items are more likely to cause diarrhea and others more likely to cause constipation?
katescarlata
This is an interesting question and I am not sure it’s a one size fits all. There are a few things that occur in the body. For one, there are many, many different gut bacteria–the bacterial composition is variable person to person. Bacteria that produce methane are associated with slowing the gut down while hydrogen producing bacteria seem to speed up intestinal transit time. When looking at methane vs hydrogen production in a breath test–those with higher methane levels tend to be more constipation predominant. Those with higher hydrogen levels tend to be more diarrhea predominant. THEN there is the factor of the food itself in the intestine. The smaller the chain of carbohydrate the quicker it is fermented by bacteria (fructose is the smallest FODMAP) and the longer the carbohydrate chains seem to have a greater impact on diarrhea than the smaller chains FODMAPs–but this is based on one small study, I believe.
Austeja T
Hi there,
could you please give a link to the study about methane and hydrogen being related to the form of IBS?
Do you maybe know if different probiotics can increase methane or hydrogen levels selectively?
katescarlata
I am not sure I understand your question. Methane and hydrogen production in the small bowel in elevated amounts may be related to small intestinal bacterial overgrowth–in this condition–antibiotics are used to reduce production of those gases.
meredith
I’m new to this diet it was suggested by my gastro.
How long till you feel it’s effects?Also I’m confused when it comes to sugar.Is it ok in moderation?I’m an x-smoker and need something but… suger free is out
katescarlata
Meredith, good to hear from you. The diet can have immediate effects for some and may take up to a week or two.
Maltodextrin as far as we know at this time is okay. If you need a mint or candy, try one with sugar only not high fructose corn syrup or sugar alcohols such as sorbitol, mannitol or xylitol. Altoids have some products that work.
meredith
thanks for the fast response on my question.My dr literaly handed me a paper and sent me on way,and I’m still waiting to hear from rd.In the mean time any ideas on putting together basic staples of the diet(no dairy)as well It’s very overwhelming.I find myself getting very frustated and starving! Your shopping list has been a big help
katescarlata
Meredith:
check out my menu and snack ideas here :https://blog.katescarlata.com/wp-content/uploads/2011/05/FODMAP-friendly-Menu-ideas-june.pdf
NOT all will be dairy free but you could try rice milk in place of lactose free milk.
Wendy
My son’s pediatric gastro did the same thing. Handed me a list (which from all my research appears to be incomplete, outdated and wrong) and shooed me out the door – told me we used our half hour of time. After the thousands of dollars of tests (all normal) I think we should get the time we need!
Not pleased. But trying. Your website has been a life saver from shopping to cooking this last week.
So, he’s thirteen and not wanting to be sick (D 10-12 times a day) but not wanting to make changes either. He is thinking little “cheats” won’t matter. He is already tired of me nagging at him. I’ve spent a couple hundred dollars last weekend just shopping for him to get started, so he doesn’t feel as deprived.
So far, so good. Except – he hates, hates, hates the Lactaid milk. I got the 2%. Any other ideas? Mostly for his cereal. He felt like if he could have cereal, life could go on.
(Apparently my spaghetti sauce could be better too lol! It’s a new life with no onion and garlic here.)
katescarlata
Wendy–Try the Organic Valley lactose free milk. I like the taste of it much better. If not–perhaps try rice milk. The Rao’s sensitive formula marinara is popular with many of my clients–you might try that too!
Theresa
FAIRLIFE milk is lactose free, has twice amount of protein, half of the carbs, tastes like regular milk – it is cows milk. It’s delicious!
Linda
Fody Olive Oil Shallot Infused, and Garlic Infused oils have made cooking and eating fun and delicious again; used in salad dressing, added to hamburger patties, brushed on roasted salmon! I switched from almond milk to rice milk and actually like it.
Samantha Matete
Hi Kate, I have a question about sugar and sugar alternatives. Is brown sugar, raw sugar and golden syrup low fodmap? I’m not a white sugar person (our family call it white death, lol!)and pure maple syrup is hideously expensive here in New Zealand. I like to bake more specifically gluten free baking and have come across a few recipes using pure maple syrup so I’m hoping a can replace this with golden syrup.
katescarlata
Yes you can sub in golden syrup for maple syrup. Brown sugar is okay too. And as far as I know, raw sugar should be okay too!
Samantha Matete
What about rice malt???
Samantha Matete
Great thanks for that!
katescarlata
Rice malt syrup is low FODMAP.
Samantha Matete
thanks again my go to fodmap guru adviser!!!
katescarlata
🙂
ALEX
Hi Kate! I hope you are doing great!
I have a few small questions… again 🙂
1. Have you done the raffle for those peanut books?
2. After elimination diet, what are the key foods from each group to start reintroducing and what’s the procedure in general?
3. Is home made popcorn ok? I guess only a small portion, if knowing that corn thins are allowed just one per sit?
4. Any news on Sprouted Corn Tortillas?
5. Any idea about Jícama? or Cactus (“nopal” in spanish)? I don’t mean prickly pears.
Guess just that…
Again thank you for your amazing patience and continuity and updates from your blog!! I already bought the PDF’s and they are huge help!!
Best wishes,
Alex
katescarlata
Yes, I did the raffle for the peanut butter give a way and cookbooks. I posted the winners on a subsequent post. Logan was the grand prize winner from Canada! Yay Logan!! I will do some other give-a- ways soon…. 🙂
So happy to hear the you have found my e-booklets (cookbook and menu plans) helpful. For those of you interested–>http://www.katescarlata.com/fodmap.htm
The elimination phase is a whole process–It would take too long to detail on the blog. But in general you stay on your low FODMAP diet and test each FODMAP group. If testing lactose, you would consume your low FODMAP diet and add 1/2 cup-1 cup of milk to one meal. YOu would do this for 3 days if without symptoms to fully test your tolerance to lactose. Fructose malabsorption or tolerance would be tested using 1-3 teaspoons of honey or 1/2 of a mango. BUT really this is best undertaken with the guidance of a dietitian….a bit long of a process to type of here. A couple cups of popcorn should be fine. No info on sprouted corn tortillas–though I do allow with my clients, no info on jicama, or cactus.
Alex
Thank you for the quick reply!!
I know all this would be better with a dietitian… But I can’t go to one for the moment. I’m seeing GP again next week on Friday where I will her a class on FODMAPS and evidence inthe UK and see if this way I finally get referred to a dietitian. Anyway…
Thank you for the answers!!
What I forgot to ask, is what is your opinion on soaking overnight grains and seeds like buckwheat, oats or chia seeds, almonds, sesame ? Soaking in water or rice or soya milk….
Would soaking increase the bio-availability of the FODMAP content in those grains and therefore the same portion be “higher” in FODMAPs?? Or would this process of soaking only affect the phytic acid and the bonds to important minerals?
Thank you again for your amazing patience and dedication to this blog!!
Best wishes,
Alex
katescarlata
Hey Alex…WE know soaking legumes in water and draining and soaking (ideally a couple times or more) reduced GOS–fructans and GOS are water soluble fibers so they leach into water and some get lost with draining and soaking. In theory other food sources that contain fructans and GOS may benefit from soaking and draining but I have no information on that.
Alex
Thank you Kate.
Have a nice weekend!! It would be great I could meet you one day… To bad you are not in Florida, as I am going to US next week…
Anyway, like always, thank you for the support you give us all with your blog. This really demonstrates about how dedicated and ethically concerned dietitian you are by providing real scientific based facts that will help the public in their journeys to a healthier life.
Best,
Alex
Amy
Kate,
I am so thrilled to have found your blog! My son is just starting this diet after a positive fructmal test and years of discomfort and many tests/scopes. (I just made an appointment to see you in June since the nutitionist at Children’s Hospital did not have a great handle on this information.)
He has been on the diet for only a week, but he seems to be having MORE stomach aches. He loves fruit but I’m not sure he’s tolerating the small amounts I am giving him of the allowable fruits (bananas and berries). Are there some people that cannot handle any fruit at all?
Thanks so much for you great information!
Amy
katescarlata
Hi Amy, this makes me suspicious that your son may have SIBO-small intestinal bacterial overgrowth? Has he been tested for this? I do find the kids are less tolerant to higher amounts of fructose and often only small amounts of fruits can be tolerated. Perhaps try a couple slices of star fruit or 1/2 a kiwifruit? But would follow up with MD regarding the possibility of SIBO.
Kate
Amy
He was tested for SIBO last year and it was negative. He also seems to have trouble with products that have baking soda or citric acid and things that are high fat. Also, is corn syrup OK if it is not high fructose? Are almond milks/ice creams a good dairy alternative (he is also lactose intolerant), I have seen different answers on whether almonds are OK.
Thanks so much for your great information!
Amy
Holly
Hello,
I was just diagnosed ibs beginning of last week. Had colonoscopy & ct scan due to losing 25 lbs & diarrhea since Feb. Started Fodmap on Wed. Tried russet baked potato on Sunday. I only had 1/2 & no skin. I put lactose free margarine on it, salt & pepper. The other foods I had before & tolerated. I was bloated & very uncomfortable after. Would it be worth trying other kinds of potato? I am getting tired of rice.
Thank you,
Holly
katescarlata
Hi Holly, the potato would not be a FODMAP issue but certainly you could try another variety to see if you tolerate it–are you working with a dietitian? Have you been tested for small intestinal bacterial overgrowth? You could try quinoa as another low FODMAP option or GF pasta such as brown rice pasta, quinoa etc.
Holly
Thank you for the reply. I am meeting with my pcp tomorrow. I just received the results last week. Depending on where this goes I was thinking of seeing if I could meet with Patsy Catsos where I am in Maine. I am 1.5 hrs from her. They haven’t tested for the bacterial overgrowth. I will mention that to my pcp. Thanks again!!!
katescarlata
Amy, corn syrup should be okay if not HFCS.
katescarlata
Holly, YES…I would recommend you drive the 1.5 hours to see Patsy! I just was on the phone with her…we collaborate quite a bit with our work on FODMAPs.
Jill
Love your blog!!! Wanted to find out about brown rice. I’m hearing two messages where some say its ok and then not. So far I’m good with white rice. Thank you so much for this info!! 🙂
katescarlata
From a FODMAPs perspective, brown rice is fine. It only has a trace of fructans-not enough to be an issue. It’s more nutritious than white and gives a bit more fiber.
Jill
Thank you so much!! I have ulcerative colitis & found that this has been the only diet that has relieved me from symptoms. I’ve tried SCD with no luck but this worked in just the first week. I know it’s recommended to add Fodmap foods back eventually after the 5-6 week period to determine the trigger foods but I was curious if you know of anyone that has remained on the diet longer or even ongoing? It seems to be healthy enough but wanted to check in.
Samantha Matete
Hi Jill, I’m commenting on your query you made a day or two ago – “I know it’s recommended to add Fodmap foods back eventually after the 5-6 week period to determine the trigger foods but I was curious if you know of anyone that has remained on the diet longer or even ongoing?” – well I have, due to the permanent damage of my digestive system from years of being misdiagnosed. My digestive improvement was so predominant from being on a strict low fodmap diet that it has lead my dietitian on a professional quest on the fodmap diet and helping IBS suffers. I can tolerate small things every now and then like tamari but have to avoid all onion, garlic, beans, legumes, gluten, high fodmaps fruit and veges, even those that say 1/4 cup is ok I still have to avoid. Its been hard and a huge adjustment but once you realise all the things you can have and adjust to clean eating and using simple food seasons like just salt, pepper and fresh herbs, not only has my digestive problems near gone but I can appreciate the taste of real food! Tho dinning out can be abit of a stress, I usual stick with a plain nice piece of steak, baked potato with butter and a simple salad. You would be surprised how chef’s react to a request like that and appreciate a eater of clean simple food, they still put their twist of chefiness on the side tho!
Jill
Samantha, you’re awesome!! Thank you so much for your reply. I can totally understand simple eating. I think I’ve tried every diet out there for digestive issues & this one is so promising so far that it’s nice to know this could be an ongoing option for some. It’s definitely better than eating just rice & bananas back in the day that’s for sure. This seems so much more flexible although I know that may be difficult to imagine in the beginning. I’m happy to hear you’re improving 🙂 many thanks again! It’s nice to hear from those going through the same steps. Take care & be well,
Jill
katescarlata
Thanks Samantha for sharing your thoughts. I absolutely LOVE when you all provide feedback and insights!!
Krista
This blog is amazing – thank you. I just found it today. I am new to FODMAPS (as of yesterday) and from everything I have read I am feeling very overwhelmed. I have IBS (relatively new diagnosis)and I am frustrated. Where can I find out more about the elimination phase and could someone possibly point me in the right direction as to where to start.
Thank you so much!
katescarlata
For my clients, I use my ‘checklist’ found in the FODMAP basics section of my blog for the elimination phase. For more specific instructions, check out Patsy Catsos book, IBS free at last on her website: ibsfree.net I also have a cookbook and downloadable 3 weeks worth of meal ideas on my website-link here: http://www.katescarlata.com/fodmap.htm
Krista
Thank you so much!. I have been trying to follow FODMAPS for 3 days and I feel a bit better already. Im curious though. It seems that everyone who talks about their IBS has IBS-D mine is IBS-C will the food maps still have the same effect?
Thanks
katescarlata
Krista, the low FODMAP diet will help with the gas and bloating but with IBS-C be sure to drink plenty of water and add enough low FODMAP fiber sources (chia seeds, strawberries, white potato with skin, oat bran…)
katescarlata
Jill and others:
Just a key point with the low FODMAP diet–it truly is a learning diet. The diet is not designed to follow long term. In fact, FODMAPs in the diet increase healthy bacteria in the gut. The bifidobacteria counts decline on the low FODMAP diet and these bacteria produce butyrate which is linked with reducing our risk of colon cancer. We all have our own balance of bacteria–so undergo the challenge phase and try to incorporate back FODMAPs that don’t trigger your symptoms.
Samantha Matete
I absolutely agree with Kate and my diet has been a long trial of introducing certain foods back and the results were of ‘those’ god awful symptoms returning. My digestive system is very damaged and highly sensitive to these fodmap foods. Also all of this has been under the guidance of my dietitian and doctors.
Jill
Hi Kate, thanks so much for this detailed information. It’s very helpful. After the initial first stage, I’ll see which Fodmap foods agree with me. Again, thank you for this beautiful and beneficial website. 🙂
Jennifer
Cocoa powder is a fodmap source? Say it isn’t so. I need chocolate. I throw it in my smoothies. I need chocolate. Did I mention that?
katescarlata
perhaps small amounts of cocoa will work for you….we all have our own threshold. FODMAPs are healthy foods overall….so you want to fit in what you personally can tolerate.
Allyson
So you may have answered this in the comments above, but truth be told…..I didn’t read all of them. I have been gluten free for 2.5 years to help with IBS and recently have cut down on dairy, primarily cream and milk. I have been drinking unsweetened plain almost milk in place…is this okay for a low FODMAP diet? I have tried coconut milk, and really do not like it. I have not tried rice milk though.
Thanks! I subscribed to your blog and look forward to filtering through it!
katescarlata
Allyson, did you mean almond milk? Want to comment properly on your question. Kate
Allyson
Yes I did mean almond milk! Thanks!
katescarlata
I hope to learn more about almond milk –I know the Australian’s were testing it…but I have not heard yet if it is low or high FODMAP or inbetween….more to come on that. For now, I recommend avoid it.
Samantha Matete
Did I catch that right…..that cocoa powder just plain 100% cocoa powder is a high fodmap food???
katescarlata
Don’t panic Samantha, if you can tolerate small amounts of cocoa go for it==our tolerance to FODMAPs do vary…BUT it appears that cocoa powder is higher in FODMAPs but chocolate–dark, semi sweet seems to be okay.
Samantha Matete
Oh thats could I seem to be fine with it. I replaced coffee with cocoa powder for my cuppa in the morning as coffee may have been contributing to my IBS and the only chocolate I eat is 70% cocoa or darker, its the best!!!!
Naomi
Just want to say Hi, fellow sufferer here, but i was recommended fodmap based on my IBD .. i am currently being treated for colitis. and finding it extremely hard to keep to fodmap when my chef partner wants to use and make things i can’t eat( he never covered fodmap in school) . how do i live my life as normal as possible , i’ve noticed everything i want to eat virtually has fodmaps in it. i’m starting to think i need to make everything from scratch, it’s doing my head in and i haven’t even had the ‘ breath’ test…. so i’m wondering how accurate my specialist is… sigh. so much to learn!
katescarlata
Hi Naomi–glad you stopped by my blog and introduced yourself–the low FODMAP diet is designed to use for the short term — 2-4 weeks and then try to add fodmaps back and evaluate whether they cause symptoms. If you go in with the idea that it’s a short term diet–it might feel a little less cumbersome! It is easy to become overwhelmed-lots of contradictory info on the web and it is extremely helpful to get help from a knowledgable dietitian.
Samantha Matete
I’ve come across another food I’m puzzled about. Is bacon a low fodmap food?
katescarlata
Bacon would be low FODMAP but of course don’t over do it….it’s yummy but not particularly healthy.
Samantha Matete
No its more of an occasion food for me! What about ham etc?
katescarlata
Samantha, the meats tend to be low FODMAP == remember-FODMAPs are carbohydrates and meats are mostly protein and fats.
Samantha Matete
Yes thats right! Its the additives that is put into them eg. gluten that I need to worry about. Thanks Kate.
jessi
ive been having so much trouble with my ibs, will the fodmap diet also help with the weight i have gained?
katescarlata
Sometimes it does seem to help with weight management. I wonder if this is due to changes in gut bacteria. Some bacteria are better at getting calories out of our food.
Jo
Hi Kate,
could you tell me please would the “Phloe Bowel Health” capsules, & Clinicians Flora Restroe Oral Probiotic cause a problem? Also, I have been eating Gluten-free bread, but some brands tend to cause more of a problem. Could it be due to the yeast content? I also find it hard to get sufficient protein throughout the day, as I don’t tend to always like to have meat, & also eggs tend to cause me problems. I used to use protein powder, but of course this contains dairy. Any suggestions? Thank you for your help.
katescarlata
Hi Jo, I am not familiar with those probiotics…feel free to send the full ingredients list and I can take a peek. Some gluten free breads have other FODMAP ingredients so be sure to read labels carefully. Gluten free does not necessarily mean low FODMAP-avoid chicory root (inulin), honey, agave, fruit concentrates. Eggs can cause issues for some people…not sure if its a sulphur issue there. Not all protein powders have lactose…there are many made with brown rice–sun warrior has an option. You could try lactose free yogurt, hard cheeses for protein or peanut butter is low FODMAP too. Canned chickpeas are allowed in 1/4 cup portion or 1/2 cup canned lentils.
Brittany
Hi Kate,
Thank you *SO* much for this wonderful resource and the work you do. I have a personal experience to relate about cocoa powder, but first a quick run-down of my story:
Several years of digestive issues have now become very chronic, acute and disruptive. I tried many supplements, acupuncture, etc., avoided wheat, dairy and corn…but kept getting worse.
My acupuncturist ordered a stool test, and I had a troublesome amount of Klebsiella oxytoca! Unfortunately, my acupuncturist didn’t really advise me. I didn’t know what to do and didn’t have insurance…had an MD doctor who doesn’t trust those sorts of tests say it didn’t necessarily mean anything. I let it go.
I finally got insurance recently and found an ND/RNP to work with. We tested for Celiac & H. pylori…both negative. I’d shown her my lab test that showed K. oxytoca a couple years back, but she wanted to try the standard elim diet before investigating SIBO.
Well….that standard elim diet nearly killed me! I may be exaggerated a bit but…not much. All of my symptoms, all the time, at 100% plus new ones I didn’t even have before.
Desperate, I spent hours combing the internet, trying to find out what the hell was happening to me. Enter FODMAPs…and your blog 🙂 I can’t tell you what a miracle/relief it was to find a list of FODMAPS foods…and to see that my diet on the elim diet was 90-95% composed of FODMAPS foods! Holy cow!
Unfortunately, the experience has me in a serious tailspin, where I spent nearly a week in bed, barely eating. But, having taken out FODMAPS foods, many of my symptoms have become more bearable.
Right now, I’m doing a combination of the SCD, FODMAPs *and* the Paleo Autoimmune Protocol…and it is SO hard to find things to eat! I just keep telling myself that this is temporary….and that I *can* get better.
ENTER COCOA POWDER. Today….I just wanted something that was a treat. I’d seen on the SCD forums that cocoa powder was okay in a sense, but not legal because of its addictive potential, which I suppose could set off other food cravings. I didn’t check carefully enough and in a moment desperate for a treat, I ate about a tablespoon of plain ole, 100% cocoa powder.
And today was one of the worst days I’ve had since going off FODMAPs. It was truly, truly horrible! I was almost instantly lethargic, terribly thirsty, extremely bloated and had a prickly feeling all over…and couldn’t sleep. It took nearly 8 hours for it to pass.
I’ll miss you cocoa 🙁 We’re like star-crossed lovers. I did read that dark chocolate may be better tolerated, esp. the less fiber it has (the fiber is the cocoa solids). Perhaps I can have small reunions with chocolate in a year, when my gut is healed.
If you’re like me, and you’re in the early stages with some complex issues….please be careful with the cocoa!
Thanks again, Kate 🙂
katescarlata
My pleasure Brittany. 🙂
Patty
Hi, I’ve just bumped into your blog and find it so helpful. There’s plenty of valuable information on FODMAPs and I would like to sincerely thank you for sharing all this! I have IBS and want to try the FODMAP diet. I understand I should first start with eliminating all high FODMAP foods for 3-4 weeks, and then add them back to find out which ones may trigger –or aggravate– my IBS symptoms. But how to proceed exactly in that 2nd phase? ie. should I add back each type of food 1 by 1 for a week each, for instance ? Any clarification on this would be greatly appreciated. Also, how long should be phase 1, that is how do I know when to start phase 2? Many thanks for your precious help! Patty
katescarlata
Patty, Yes, you follow the low FODMAP diet for 2-6 weeks in general–hopefully your symptoms settle down in this time frame. The re-challenge phase involves adding back FODMAPs by their FODMAP groups–fructose, lactose, fructans, GOS, mannitol and sorbitol. Here is a short but sweet recap….
Choosing a food with ONLY that FODMAP when testing that group. A fructose challenge would involve staying on the low FODMAP diet and adding in 1/2 a mango OR 1-3 teaspoons of honey and evaluating your tolerance to the added fructose food over the course of 3 days. If you experience IBS symptoms you can assume that you are malabsorbing fructose at this time and it is contributing to your IBS. YOu would avoid the excess fructose containing foods and move on the the next challenge such as lactose…. Tolerance to different FODMAP groups can change over time so re-trying the challenge at a later time-say, 3 months is a good idea.
Patty
Many thanks for your precious feedback, Kate. It is much clearer now! Yet, I have one more question about phase 2: if I add back half an apple for instance, how do I know what FODMAP group it belongs to as I seem to understand apples belong to the Fructose, Fructans and Polyols groups? If IBS symptoms come back when eating that half apple, would that mean I have problems with foods from those 3 groups??
katescarlata
Patty, You would never use an apple as an initial test food as it has more than one FODMAP group. Perhaps you could test sorbitol then fructose and if you pass both…perhaps try a 1/2 of a granny smith or pink lady apple which only these 2 FODMAPs. Perhaps start with 1/2 medium with skin on and then titrate up if with good tolerance.
Shirley
I found a powdered peanut butter called PB2. You just add water to it to make peanut butter. It is 2 Tablespoons of powder and aprox. 1 tablspoon of water or more to get the desired consistency. The peanuts are slow roasted and than pressed to remove 85%of the oil. Calories per 2 tablespoons is 45 cals and fat cals are 13% This might be a good product for people that need to restrict fat and oils.
Web site for this product is bellplantation.com
katescarlata
I do love PB2==it shouldn’t be an issue for FODMAPs as peanut butter is okay…but altering the state of food can alter FODMAPs so just monitor tolerance.
Christine Robinson
Hi Kate,
I recently found your blog/website and it is wonderful! I am an RD in LTC and am on the planning committee for the MA DHCC group. Would you be willing to give a talk about this dietary approach to our group in September?
katescarlata
Hi Christine! I have 2 talks scheduled already for September. What date are you looking at?
Christine Robinson
We are looking at Sept 19th but don’t have our venue booked yet.
Kristine
Hi! Great homepage! I started om my FODMAP diet last Friday, and already getting better. Don’t look pregnant anymore…!
I have tested negative for lactoseintolerance, so I could acctually include lactose in my diet – but my dietitian wanted me to exclude it in the start. Have you any experience in that issue? People testing ok for lactose, but still experience low tolerance? Have you tried Erythritol? I can not find this togehther with sorbitol, xylitol, mannitol… I see it is a -ol sweetener, but can not find out if this one causes problems..
Thanks in advance!
Regards fro Norway 🙂
katescarlata
Hi Kristine all the way from Norway!! I think in some cases its a good idea to do all the dietary restrictions on the low FODMAP diet just in case the testing was inaccurate. You can always test your tolerance to lactose via a dietary challenge later. Erythritol is generally well digested unlike the other polyols but I did just read a study that suggested fructose when combined with erythritol made symptoms worse…so I would avoid in you can. Here is the link to the study: http://www.ncbi.nlm.nih.gov/pubmed/22118754
Patty
Thanks a lot, Kate. It is crystal clear for me now! Enjoy your day! –Patty
EdithB
Dear Kate, Thanks for your clear summary of foods to eat and avoid, it’s a great help. I apologise in advance if this is on your chart but I was wondering where cream stands regarding FODMAP content or if there are differences between single/double/whipped?
Thanks!
katescarlata
Edith, Whipped cream is allowed in a 2 TB portion on the Monash App. I don’t have data on double or single but I believe it is similar to our whipping cream and light cream which should be okay in small portion 1-2 Tablespoon (US) but not in large serving.
Darlene Palladino
Hi, Just started with FODMAP foods. I love Ezekiel breads are they allowed? Also romain lettuce. I Have microscopic colitis with IBS-D. Your blog is GREAT. Thanks
katescarlata
Darlene, romaine would not be a FODMAP issue but not sure how it will impact your colitis. I find the tender leaf lettuces to be better tolerated: butter (Boston, bibb), or baby spinach or arugula. Ezekiel breads at this time are not allowed. We need to evaluate them–sprouting grains should make them easier on digestion…but not enough info on this yet. And thanks, I am happy you like my blog! 🙂
Dar
Thanks for your reply. I am wondering what large chain carb foods are. Thank for your help.
katescarlata
Darlene, larger chain carbohydrates include starch and fibers that are much longer in length than SHORT chain FODMAPs. Starch is digested in the small intestine completely while fibers and resistant starch are not digested in the small intestine but rather help with normal function of the large intestine and formation of stool.
Dar
clear and natural metamucil is recommended as a fiber supplement but it is veg inulin. Inulin is on the do not us list for fodmap foods. can you help with this. also is sourdough bread ok i am getting two different answeres. Thanks
katescarlata
Dar, I would not recommend an inulin based fiber supplement on a low FODMAP diet. It’s easy to get enough fiber on the low FODMAP diet–just 1 Tablespoon of chia seeds has 5 grams! Here is some additional high fiber low FODMAP foods to incorporate per personal tolerance: https://blog.katescarlata.com/fodmaps-basics/fiber-without-fodmaps/
Adding sourdough starter to breads does seem to break down the FODMAP content–I have not seen much data on this-just one study evaluating grains done by Monash University. On the elimination phase I would avoid all wheat, barley and rye based breads—when you do the challenge phase perhaps try your tolerance to a white sourdough bread. Many of my clients tolerate sourdough breads in one serving size portion.
Dar
Could you recommend some tea or herbal tea that are safe. Your web-site is fabulous so much info. Just wonderful.
Dar
I wonder if anyone out there has tried the butternut squash bread. I did this week-end and it failed.
nadine
hi kate..i am wondering about the reintroduction phase..we reintroduce weekly each category? must we have a break period between each?
katescarlata
Nadine, I think if you develop symptoms with a particular challenge then you should wait until you are symptom free for a few days before undergoing a new challenge. Otherwise, it’s not really necessary to wait too long between FODMAP challenges…
Matt
I love sweet snack foods and I am trying to start the FODMAP diet. I came across this website with glutin free snacks. http://www.glutino.com/products/cookies-and-wafers/
Are any of these low FODMAP? I know there are questions about chocolate but are the vanilla or lemon cookies low FODMAP? I don’t see HFCS but don’t know about some if the sweeteners. I would really appreciate you opinion.
katescarlata
Not positive Matt on the cassava flour but I think they may be okay. When it comes to reading labels, avoid soy flour, bean flours, molasses, high fructose corn syrup and other more obvious FODMAP sources. Also, chicory root extract (inulin) that is added to SO many products.
Keep cookies at a minimum (2) per day and try to stick with real foods while on the elimination phase.
Samantha Matete
Hi again, do you know if gherkins are a low fodmap food?
katescarlata
Hi Samantha, Depends on the brand. Some are made with high fructose corn syrup. DelMonte brand looks okay from what I found on shopwell.com but Heinz did not.
Samantha Matete
Ok so I should just check the ingredients list on the brands here to see if HFCS has been used….if not then ok?? I was asking as I like gherkins but also they are used in tartare sauce….
katescarlata
I think HFCS would be the primary potential FODMAP in gherkins.
Jennifer Page
Hi Kate-I found your blog while searching for help for my daughter. She has been diagnosed with SIBO and FM and I am having trouble navigating through the FODMAPs. It seems like I have it figured out, then we spiral out of control again. I can’t keep weight on her. I would love to work with a RD that knows about FODMAPs. Do you have any colleagues in California? Thanks…
katescarlata
Hi Jennifer, Yes, I do have colleagues in Cali–where are you located?
Jennifer Page
We live in Murrieta, Ca. South of Riverside, north od San Diego.
Jennifer Page
We live in Murrieta, Ca. South of Riverside, north of San Diego.
katescarlata
Jennifer: I recommend EA Stewart–she is very knowledgable in FODMAPs! Her website is: http://www.eastewart.com
Sandi
Thank you for your blog! My 13 year old son is lactose intol and I just found out about FODMAPS. WHy hasnt any MD ever mentioned this??? He suffers with diarrhea, stomach nausea/cramping/fullness all the time. He just fell to the 1 percentile for weight for his age. Just started with a RD, but not confident with her knowledge. Im desperate on how to try and get some weight on him! We live in NH. His appetite is poor. I just bought BOOST, but then saw although it is lactose/gluten free, it has soy….is that OK? HELP!
katescarlata
Sandi,Glad you stopped by my blog! First of all be sure your son has been screened for celiac. That should be done first with a blood test for initial screening. The other test that I think is very important is a breath test for small intestinal bacterial overgrowth. This occurs when bacteria from the large intestine sneak into the small intestine and contribute to bloating and cramping. Boost “should” be low FODMAP by ingredients listed–the soy ingredients are soy protein isolate and soy lecithin which do not contain FODMAPs. The soy we minimize on the low FODMAP diet would be soy flour, edamame, or products made with whole soy beans not soy protein isolates. (the exceptions, tofu and tempeh which have been found to be low in FODMAPs due to processing even though they are made with whole soybean). In general, I am not a big fan of supplemental drinks. The reason being is that the Monash University researchers have analyzed similar products that are used in the hospital setting in tube feedings and found that despite low FODMAP ingredients being listed –the products when tested, where high in FODMAPs! Makes me wonder what is in some of these supplements!
If you want to try small amounts of boost–say 1/3 of a serving you son may do better with it rather than a big dose all at one sitting. There are dietitians in NH that are well versed in FODMAPs–perhaps you should seek out another RD to work with? As for why doctors don’t mention FODMAPs….So many of them haven’t heard of it yet…or are just hearing the buzz about this diet. I have been on a mission to get the word out…we can all take a part in educating others!
Sandi
Thank you, thank you, thank you for being a life line in this! Celiac, Chrons and IBD were ruled out by endoscope/colonoscopy. Is almond milk OK or should I have him use lactaid in his gluten free cereal (chex) and when I cook/bake. How about Earth balance buttery spread that is gluten/lactose free and non gmo? Im feeling scared that though the RD is looking at food sensitivities, he is still only 73# and 1% on the weight chart. So hard to figure out what is ok for him, but try so hard to get him to actually gain some weight too! There are a lot of products that substitute soy for lactose. Remind me again what is ok, and what is not? Soymilk? Thank you so much for your help!!
Sandi
What about chocolate? It seems that a lot of lactose/gluten free treats are always covered in chocolate? Kevin likes the so Delicious brand non dairy/soyfree treats, but they all have chocolate?
Sandi
what is the treatment if the breath test reveals SIBO?
katescarlata
Treatment for SIBO is an antibiotic. I believe the low FODMAP diet can be beneficial as well. meal spacing….eating every 3-4 hours instead of grazing. It’s individual–working with an RD and doctor that has experience with SIBO is very helpful.
katescarlata
Sandi-Although they taste yummy, many of the So Delicious products don’t fit the low FODMAP diet. Many have agave syrup or chicory root extract added. The almond milk products are not OFFICIALLY off limits but likely will be once we learn more from the Monash researchers–almonds have a high amount of GOS one of the FODMAP groups. So only 10 almonds are allowed with in the ‘cut off’ for GOS amount. Since GOS are water soluble fibers –they likely leach into almond milk when it is being made. I know, this diet is complicated….but it gets easier the more you learn!
Sandi
is there anyone in vt/nh that you would recommend?
katescarlata
Sandi, check the dietitian registry on ibsfree.net and see if you find a dietitian close to you. I can’t vouch for all the RDs listed…but its a good starting point. You might want to ask to speak to the dietitian prior to your meeting to get an idea of how well he/she is versed in the diet.
Jennifer Page
Kate-One of the struggles I have is narrowing down which food is the “offender”. Does the FM reaction of gas/abd. pain and cramping result immediately after the offending food or 12 hours later?
katescarlata
Jennifer, that varies from person to person–most of my clients have experienced symptoms within 3 hours. For more constipation predominant patients it may take longer.
Samantha Matete
Would under 100ml of milk be enough to cause bloating? As you know I have been following the low fodmap diet since January, just recently I bought normal milk instead of the lactose free milk, the rest of my diet has remained the same so I’m guessing this is causing my severe bloating! My tummy is sticking out so much though I have no excessive wind or pain just this huge bloated stomach! The amount of milk is under 100ml and I have it with my hot cocoa (1 tsp plain cocoa powder and a little sugar) with my breakfast of kiwifruit, cooked brown rice and homemade natural yoghurt. I just feel I am always on a constant battle with the bloating I get no matter what I do or eat!
katescarlata
Samantha–you may be very sensitive to lactose –100 ml of milk could have 5 grams of lactose–also in case you missed my post about the Monash updates or my most recent post: COCOA is high FODMAP too so perhaps the combo of milk and cocoa was too much. Is your homemade yogurt low lactose? That too could be an additional issue.
Samantha Matete
Well I’m now guessing that I am sensitive to lactose. Making your own yogurt allows you to let it culture for at least 24 hours, the long 24 hour fermentation ensures that all the lactose in the milk is used up. And I can still have those important probiotics in my diet. So I’m unsure about cocoa. I replaced coffee with cocoa as my dietitian said that coffee can upset IBS. I never really had a problem with cocoa before. I eat dark chocolate and I think thats been ok. I’m thinking that it is my breakfast meal thats upsetting me. The rest of the meals I have under control and adapted well. What I’m trying to do is convert or adapt with my morning meal to include fruit and protein. I always have kiwifruit, its my fav fruit plus its really helped control my constipation and I have found that the morning is best time to get my fruit intake. Its also important for me to have protein with everymeal so thats why I have been using lactose free milk and yogurt with the kiwifruit and brown rice but now I’m not sure that is the best. I tried adding seeds in my rice and fruit but that upset me. I’m thinking that I should just avoid the milk and yogurt now altogether and now cocoa so what the hell can I have for breakfast. Perhaps I will just eat my kiwifruit on its own first (I used to chop it up and have with my rice and yogurt) then have my rice with an egg (I found out that its not only ok but good to eat an egg a day) and tea. What do you think?
Samantha Matete
Ok just did abit of research…..I’m suspecting that it is the fruit, as well as the yogurt and cocoa, causing my bloating. It seems to be foods that I eat that cause fermentation in my gut that causes the bloating. “Fruit should be eaten alone or with other fruit on an empty stomach. This is because when fruit is eaten, the digestive process works very quickly and our body uses different enzymes to digest the fruit. The simple sugars contained in fruit need time to be completely absorbed by your body. When fruits are eaten alone, your stomach can more easily process all of the nutrients, fibre and the simple sugars contained in the fruit. The best time to eat fruit is first thing in the morning on an empty stomach”.
Samantha Matete
is tofu low fodmap? confused as soy is a high fodmap. also I do not tolerate any beans and legumes and their products so would I be ok with tofu and why? also what about miso?
katescarlata
Tofu is considered low FODMAP by Monash researchers. Some tofu products may be a problem such as silk that are prepared and thickened in a process that does not involve draining the FODMAPs and liquids away from the protein part of tofu. But extra firm traditional tofu should be okay (low FODMAP) I can’t say whether you might have an issue with tofu…we are all different. Miso is not allowed on the low FODMAP diet at this time. I have not seen any info suggesting that it is low FODMAP.
Samantha Matete
Thanks for the reply and info. I have been doing some research on fermenting foods and wonder what your thoughts are on this? Are they fodmap friendly (obviously using low fodmap veges)? This is one of the sites rather convincing for helping digestive troubles and conditions like IBS. http://www.spiritofhealthkc.com/portfolio/fermented-foods-history/
katescarlata
Samantha, I think fermented foods can be a healthy addition to our diet. I like my clients to add yogurt (lactose free if need be) to their diet and some kimchi, if they like it. NOT all yeasts or bacteria added to fermented food offer probiotic or beneficial effects though. But many fermented foods are made with probiotic yeast and bacteria so may in fact be helpful. It’s true that bacteria can help break down some of the difficult to digest carbohydrates making it easy for our body to absorb the food better which leads to less gas and bloating potentially. I do think there is a fine line with use of probiotics and probiotic fermented foods…. that overfeeding the body probiotics may do more harm than good for some people with IBS. There is the possibility of too much of a good thing. Just my perspective.
Caitlin
I had another question about fermented foods. Is kombucha allowed on the low FODMAPs diet? What are your thoughts on kombucha?
katescarlata
NOt yet tested. In theory–fermented foods should lower FODMAP content.
katherine
Metamucil, yes or no?
katescarlata
Katherine, this is an excellent question! Metamucil markets a variety of products so when you refer to Metamucil you need to know what product you are looking at….Metamucil clear is 100% inulin–NOT a FODMAP friendly product. Other metamucil products are psyllium based which for some IBSers, a tolerable fiber source. Read ingredients on all fiber supplements…some varieties are sugar free and have mannitol or sorbitol– these sugar alcohols are FODMAP sources as well. My favorite fiber supplement: Chia seeds! All natural, nothing but chia. 1 Tablespoon has 5 grams of low FODMAP fiber. Compare that to a metamucil or citrucel caplet that has a whopping 1/2 a gram of fiber! Chia can be found at Whole foods or even many main stream grocers. They can be sprinkled on lactose free yogurt, on top of a salad, in a smoothie, on top of oats.
Jennifer Page
What is your opinion on Stevia?
katescarlata
Stevia I believe is fine on low FODMAP diet–not sure how it is for gut bacteria or health in general. Products made with stevia often contain sugar alcohols so be careful when selecting your product.
Martine-Aimee
Good morning Kate,
I recently purchased your 2 books (recipes + 21 days). I would like to follow the 21 day plan perfectly. However, I live in Canada, and can not find some of the products in your book (for example, Green Valley yogourt!!). I will go to the US to do this special grocery shopping. I will go to Burlington. Which big chain grocery store should I look for? Of course, I will also look up some organic food stores…
Thank you for your help!
Martine-Aimee
katescarlata
Hi there Aimee, I would go to Whole Foods if possible. Not sure where there is one in Northern Vermont but check the area. I know Burlington has a great natural health store right downtown, the name I can not remember at the moment but it is well known in the area…I would imagine they have many of the speciality items I mentioned. Market Basket also has a fair amount of appropriate gluten free products that I recommend in my plans.
Dar
I have been following FODMAP for almost 2 months now feel so much better. I used to eat beans and legunes.. are there any safe ones? and what about cranberry? Your blog is great. Thanks
katescarlata
Dar, 1/4 cup canned chick peas and 1/2 cup canned lentils fall below the FODMAP cut-off. So would try those first. Other legumes can be tried cautiously when you do the reintroduction or challenge phase of the diet. From what I have read, red kidney beans are the highest. The more you soak and drain legumes, you reduce the GOS content which makes them more tolerable. Not sure that fresh cranberries have been tested as they are not readily available in Australia. But cranberry juice-1 cup (100% juice) and dried cranberries (1 tablespoon) are allowed.
Dar
I know that honey is not allowed, but is there a difference in raw honey or is it still not friendly. Thanks for all of your help.
katescarlata
Raw or not, honey is not allowed. At least during elimination phase. Some people may find honey is not a trigger and if not, then add some back.
Lesley
Hi I’ve been following the restrictive diet for a while and started to reintroduce. Low lactose, 2/3 spoons yogurt and small amounts of milk, was fine but second week 2 slices toast a small reaction then 3 brought most ibs symptoms back. I’ve cut bread out again, only 2 days now, but symptoms still an issue. Should I cut lactose out again too? It’s not clear if during reintroduction phase need to exclude ones tried again whilst trying another. I have got a referral to a dietitian but IBS not considered urgent so could be months before I get an appointment!
Thanks and lots if great things on this site which will take me a while to go through!
katescarlata
I think when symptoms flare, it is helpful to go on the full elimination diet for a couple days. Also, consider testing for small intestinal bacterial overgrowth. Some clients have difficulty adding back yogurt on a daily basis and I wonder if the presence of SIBO is part of the reason.
M.G.
At a follow-up visit this morning the specialist diagnosed IBS and recommended a FODMAP diet and Metamucil. Looking over several websites I found yours to be the most instructive and useful. Thank you for your help. Now comes the issue of finding suitable FODMAP products and chia seeds (rather than Metamucil) from grocery stores in this corner of S-W Canada where there is no Whole Foods outlet or anything similar. This is torture for a foodie whose life has revolved around ALL kinds of foods and cuisines. Sure hope to see results in short order!
katescarlata
M.G. perhaps you can purchase the chia seeds online? Metamucil is a bit tricky as there are a few different types…..stay clear of the metamucil clear which is 100% inulin! Chia seeds are a wonderful low FODMAP way to incorporate fiber. 1 Tablespoon has a whopping 5 grams of fiber! Don’t worry about buying a bunch of manufactured low FODMAPs packaged foods–stick with natural ingredients mostly: Baked potato, chicken, salad with lemon and olive oil, oats and oat bran cereal, quinoa, scrambled eggs with spinach and cheddar cheese…and sub in a few of the low FODMAP package goods to fill in the gaps. The low FODMAP diet is a learning diet….so hopefully after you restrict the FODMAPs you will feel wonderful….and then test your tolerance for which FODMAPs are your personal culprits. Different people have different sensitivities to FODMAPs. I bet you will find you can incorporate some of your favorites back in your diet!
Lauren
Hi Kate,
Your FODMAPS checklist indicates that FODMAPS should be limited to <0.5 g per sitting and to follow the limits of the individual groups. How can I find out the fructose, fructan, and polyol content of a given food? For example, if I wanted to eat cauliflower and keep the polyols to <0.3 g per serving, how would I know how much cauliflower I could eat to maintain that limit? Or would you suggest thinking about it in terms of portion size (e.g. only having a half cup serving)?
Thanks!
Lauren
katescarlata
Hi Lauren, We don’t have all the data yet to use those numbers. Cauliflower exceeds the limit so not a good one to consume. The Monash low FODMAP app does include some limits for foods.
Lauren
Thanks, Kate. I will try downloading the Monash low FODMAP app.
So, would you recommend completely staying away from foods on the CAUTION list?
katescarlata
On the elimination phase try to stick with the green lighted foods Lauren!
Peyt
Hi Kate,
Is there a source to look up low FODMAP recommended supplements? Even if basic supplements like Vitamin C or D or ….
It seems like every other supplement I buy I have to return because it causes problems… Thanks so much
katescarlata
Not that I know of….though that sounds like a well needed handout!! I will try to work on one…but might take a little time. Sometimes it can be the nutrient itself and not the potential fodmaps in the pill that bother you…calcium carbonate and iron are constipating…and magnesium and vitamin c can cause diarrhea.
Martha Coleman
Hi Kate,
Thank you so, so much for your wonderful website! I have a new case of IBS (about six months) and eating low FODMAPs foods is helping a lot. My problem is that I also have GERD. I haven’t been able to find any lists which merge low acid and low FODMAPs foods. Do you know of any? I’m finding it very challenging to get enough calories in and might find it easier if someone with more experience provided ideas for those with these two problems. It must be fairly common.
Thank you!
Martha Coleman
katescarlata
Hi Martha, Glad you stopped by…many of my clients can tolerate acidic foods despite GERD. It is only the untreated GERD patients that have a irritated esophagus that might find acidic foods a challenge–so work with a dietitian to ensure you are not overly limiting your diet.
I don’t have a list that merges low FODMAP and low acid…sorry.
Kristen Fernandez
Hi, I had a question about protein powders. I read in one of your posts that we shouldn’t really need to be adding these to our diets. I have Gastroparesis and commonly need to turn to a protein supplement, especially during bad flare-ups when I cannot tolerate most food. What, if any products would you suggest? Or what should I look for in a low fodmap powder? Thank you so much. I really enjoy your site and have recently become very interested in trying a low fodmap diet to see if it helps my GP/IBS symptoms.
katescarlata
Sun Warrior classic plain protein powder looks good. http://www.sunwarrior.com/product-info/classic-protein/ or unflavored egg protein http://www.jayrobb.com/protein/egg-white-protein-unflavored.asp Warm liquids help with stomach emptying and ginger too…though you may already know that!
Jennifer Page
Just curious, is the brown rice protein powder not a problem? I’ve been trying to find a protein powder for my son to help him gain weight, but he hasn’t been able to tolerate brown rice. Would this be different? I would love to be able to use it too! Thanks!!
katescarlata
Jennifer–the brown rice protein should be okay –I have not seen data from Monash that it has been actually tested for FODMAPs but based on what I know it should be low. There remain many grey areas for FODMAP food content. THAT being said, if you son is troubled by brown rice, I would avoid the brown rice protein or perhaps try it in small increments depending on what intolerance he has experienced in the past. Brown rice only has a trace of fructans so is low FODMAPs….but there may be some other component that troubles him in the rice.
Rebecca
Thanks for this great website! I am transitioning to Low FODMAP and have always eaten greek yogurt for breakfast. However, I have been seeing a lot in the health blogs lately about skyr, which is an Icelandic variation. It contains less sugar than my greek yogurt (4 grams for a 5.3 ounce serving) as well as four times more protein. I am wondering if skyr would be a good greek yogurt alternative for me or is it still basically the same thing? Thanks so much!
katescarlata
The plain Siggi’s yogurt by skyr looks good but some of the fruited flavors have agave which is not allowed. Strawberry and blueberry would be okay but plain is best and add your own fruit. Bear in mind the Greek yogurt’s are lower in lactose but not lactose free–if you want to try the elimination phase of the diet with lactose free yogurt and then assess your tolerance to Greek yogurt during the challenge phase that is another option. Though many of my clients can handle Greek yogurt just fine.
Rebecca
Fantastic–thanks so much! 🙂
Cocoa
I am on the week 2 of elimination and so far so good. I have a question regarding raw milk. Is it ok to eat yoghurt or curd made from raw cow milk at the elimination stage? And going by the fact that raw milk is easier to digest than regular milk, can raw milk be used in elimination stage instead of drinking the lactose free milk? I don’t mind the fat in the milk as I am looking to gain weight. thanks.
katescarlata
I would be cautious to use raw milk in my digestive health clients due to risk of food borne illness when they likely have altered immunity. Raw milk would still contain lactose so would not be allowed for that reason.
Katherine
I have dealt with SIBO, but based on recent breath tests, it seems to be gone. I’m on a low fodmap diet, but I find vegetables to be really, really hard for me. The more I try to increase my intake and include them in my diet, the more I struggle with GI symptoms (bloating, constipation). Are there some people who just don’t tolerate vegetables of any kind? I feel like I’m sort of a meat, fruit & potato kind of person.
katescarlata
Katherine, I would work with a dietitian to sort this out….everyone can present a bit different. It might be just a trial and error to see how much you can eat and what types –trying tender greens–like baby spinach, arugula or bibb lettuce maybe–and small amounts vs. Iceberg lettuce. Or perhaps you may tolerate small amounts of zucchini sautéed. If you can tolerate fruit–I would bet that with a bit of experimenting you may find small amounts tolerated.
Amy
Hi, I have been doing the fodmap diet for 6 months, it changed my life! I was cured! But over the past few weeks my stomach is just getting worse and worse. Unfortunately it feels like it’s going back to how bad it was before. Do you have any tips or advice?
Thanks
katescarlata
Perhaps follow up with a gastroenterologist and discuss the possibility of small intestinal bacterial overgrowth. A trial of a probiotic may also be helpful. But, discuss with your GP.
Sonya Mason
Thanks for your website, this has been exceptionally helpful to my Mum, who suffers from fructose malabsorption.
I live in Australia and am wondering about bread. One of the main gluten free breads sold in major supermarkets here, is called Country Life. I have listed the ingredients below for both the multigrain and the white. I’m wondering if you could take a look to see if they would be suitable.
Thanks!
Sonya
———————–
Country Life Multigrain GF:
Ingredients:
Water, Modified Tapioca Starch (1442), Rice Flour, Maize Starch, Mixed Grain (3%) (Corn, Quinoa), Linseed, Vegetable Oil, Sugar, Soy Flour, Egg White, Iodised Salt, Kibbled Mungbeans, Psyllium Flour, Yeast, Hydroxypropyl Methyl Cellulose (464), Preservatives (282), Vegetable Gum (412), Vitamin (Thiamin).
Country Life White GF:
Ingredients:
Water, Modified Tapioca Starch (1442), Rice Flour, Maize Starch, Vegetable Oil, Sugar, Soy Flour, Egg White, Iodised Salt, Psyllium Flour, Yeast, Hydroxypropyl Methyl Cellulose (464), Preservatives (282), Vegetable Gum (412), Vitamin (Thiamin).
katescarlata
Sonya, Not loving either of those choices. I bet you can find a more suitable bread with less additives. Kibbled mungbeans, too much linseed ? Fodmaps–try to find another brand if possible. The White version is less FODMAP-y but keep looking.
Anna
Thank you so much for this wonderful site! I know pumpkins are a no-go, but how about other winter squashes such as Acorn squash? Would those be OK during the elimination phase?
katescarlata
Kabocha (Japanese pumpkin) is okay…but have not seen data on Acorn.
Chris Watkins
Hi Kate,
Re honey – you said: “A fructose challenge would involve staying on the low FODMAP diet and adding in 1/2 a mango OR 1-3 teaspoons of honey and evaluating your tolerance to the added fructose food over the course of 3 days.”
I suspect this isn’t a reliable test. I’ve seen very varied figures for the GI of honey (from 40 to 87) which I’d guess is due to the varying fructose content. Makes sense as the sugar in honey comes from flower nectar, which probably varies widely in composition. The one with a GI of 87 is presumably very low in fructose and not a good choice for a fructose test.
Perhaps stick to the mango, or buy some fructose. (HFCS also no good as that varies widely.)
Hope that’s helpful… thanks for the blog. I’ve had a lot of benefit from a mostly low FODMAP diet but you’ve prompted me to do it properly and figure out for sure which FODMAPs bother me.
katescarlata
Chris–Interesting comments–ripeness of fruit can impact fructose content too! We are simply using a testing source with more fructose than glucose –only 0.2 grams more fructose than glucose quantifies something as a source of ‘excess fructose’–so it’s more about the excess fructose than the total amount of fructose.
Chris Watkins
Hmm. Not my area of expertise, but I saw an early table GI in c1985 that put fructose at a GI of 20, glucose at 100, and sucrose at 60, suggesting it effectively acted as a simple mixture of fructose and glucose. Honey was 40 (as I recall).
But (now I finally get to the point!) I later saw honey rated at 87. If that was on a similar scale, and if we assume that the dominant sugar monomers are fructose and glucose, it suggests that this particular honey is not a source of excess fructose at all, but rather a source of excess glucose.
I’ve done no lab research myself, and if the FODMAPs researchers say that honey is a valid test, then it probably is, at least usually… but more serious errors than that have been made in the name of science, so I think I’d be testing with something other than honey.
I could have saved myself some typing if I did a web search *before* commenting 🙂 http://www.livestrong.com/article/270875-honey-vs-sugar-glycemic-index/ – based on the GI, clover honey probably has no excess fructose.
Terri Sidell
Kate,
What is the recomemed portion of cooked white rice?
katescarlata
Terri–there are no measurable FODMAPs in white rice–I would just keep the portion about 1/4 of your plate or slightly more for good balance and nutrition.
Jill
Kate,
I’m looking for a low-fodmap pumpkin pie recipe. I just started with the FODMAP diet in June. I have white rice flour that has a recipe for pie crust on the back. I also have a can of organic pumpkin puree but all the recipes I see call for soy milk or evaporated milk, or even coconut milk. My gastro told me coconut milk may have too much fat for my system to tolerate. I’m allergic to almonds, break out in rash every time I eat them so I’m a little afraid of almond milk. I’ve heard of rice milk but haven’t tried it in anything yet, let alone baking. Any suggestions?
katescarlata
Jill–First we need to be sure the US pumpkin is low FODMAP. I have not received confirmation that it is–though I sent some canned pumpkin which is currently being tested. Australians call what we refer to as squash as pumpkin so it can be confusing when reading their info. I think you could sub in some rice milk in a pie filling recipe –you might use a bit less as it has not no density too it–very thin and watery. Hopefully I will learn officially about pumpkin soon…
Jill
I’m going off this chart the doctor gave me. http://lowfodmapsdiet.com/wp-content/uploads/2011/11/ListOfFodmapsFoods3.gif Based on that, I should be ok with the pumpkin. I’ll try the rice milk in the pumpkin pie recipe and see how it turns out. Thanks for getting back to me so quickly.
katescarlata
Jill– this handout is not updated and seems to be based on UK or Australia terminology –but of course you can try US pumpkin and see how you do!!
Natalie Pitaro
Kate,
This is such a specific query but I’m at wits end…..a breast fed baby who’s starting solids. Do you have any solutions for a FODMAP friendly baby purée that won’t cause constipation? I had been basing my concoctions on banana in contrast to the common apple/pear/apricot based recipes only to be told that the banana could be the cause of my little ones constipation 🙁
NB: I’m on the FODMAP path due to the change in her gasiness & bloating when I began my own FODMAP diet while she was exclusively breast fed.
Thanks!
katescarlata
Perhaps try small amounts of sweet potato puree (it has some FODMAPs when in large serving–maybe try 1-2 tablespoons) mixed with rice cereal or try a blend of sweet potato with other other low FODMAP veggies. Not sure that banana is constipating for everyone…so maybe alternate with banana.
Rachael
Hi, I have a history of microscopic colitis and ibs, noticed a big improvement with the fodmap diet. I began taking some amino acids and supplements (holy basil, astralagus, yucca, chorella) to treat my mastocytosis. Mangosteen has been he biggest help, but something is giving me fodmap symptoms and I’m not sure what (and am REALLY hoping it is not the mangosteen). Do you think it is any of the amino acids or supplements?
katescarlata
Rachael–I am not sure. I can’t find an accurate account of the nutrient breakdown of mangosteen–may be excess fructose. One option is to try small amounts spread out throughout the day vs. taking it once a day? Amino acids themselves are not FODMAPs –fodmaps are carbohydrates. The other supplements–I have no idea.
Kathy
Hi Kate. Your website is really helpful, thank you. I have a few questions re the challenge phase. I have been on the FODMAP diet for 2 weeks and was told to then challenge one food group at a time every 3rd day. I have been eating reasonable portions of 3 or 4 foods from the food group I am testing for one full day then going back to the FODMAP diet for 2 days before challenging the next group. 1) Will testing this way produce an intolerance result? 2) Should I be testing the foods for more than one day and 3) Should I be going back to the FODMAP diet for 2 days before testing the next group or do I test the next group straight after? My thinking was that I would need to go back to the FODMAP diet so if I had a reaction, I would know what group I was reacting to. I guess the big question is, is this correct or have I misinterpreted how to challenge altogether?!
katescarlata
Kathy–the re-introduction phase should be done very methodically. Foods selected for the particular FODMAP challenge should contain ONLY the FODMAP you are testing. So for fructose–it could be 1-2 tsp. honey or 1/2 mango. An apple would not be a suitable challenge choice as it has multiple FODMAPs. You test your tolerance to the FODMAP not just any food within the group. If that makes sense. This part of the testing –really should be done with the guidance of an RD if at all possible.
Kathy
Thanks Kate. My GP put me on the diet but I will take your advice and find an RD to guide me through it properly. I did make sure that I didn’t choose a food in multiple FODMAPs eg. apples and pears, though I did my Lactose challenge in one day consuming a small tub of yogurt, a cup of milk, 1.5 tablespoons of sour cream and a scoop of ice cream. After reading your reply and some more blogs it sounds like I challenged too much lactose in the one day and also should have tested over a few days not just the one.
Sarah
Hello!
I’ve been dealing with indigestion aka functional dyspepsia for many years and recently went to a GI who put me on the FODMAPS diet. I was wondering if you know of any differences in how to tailor the diet for dyspepsia vs. IBS. I had expected fiber to be an issue, but it seems like that isn’t a factor with FODMAPS. Should I be cross-checking to eliminate high-fiber foods as well?
As a vegetarian, I was wondering what soy is okay and what isn’t–tofu seems to be fine, but not soybeans? What about tempeh? Also, the FODMAPS list my doctor gave me had some differences, like eggplant is a no-way but artichokes are fine. What accounts for these differences? Is your site always the most up to date?
Thanks so much! I’m so happy to have found your site!
katescarlata
Sarah–I try to keep my site up to date and in-line with the Monash University research. Not sure why artichokes listed okay– 1/4 cup of artichoke hearts would be okay–but not full globe or jerusalem artichoke. Eggplant is okay per Monash University–the leading authority of FODMAP food analysis at this time.
So…this is the deal about soybeans–it is the water-soluble fibers in soybeans that are sources of FODMAPs–when tofu is made the water soluble fibers are drained off–or most of them. This would be different in silk varieties however–which are made differently…so I suggest you avoid Silk tofu. But firm, drained traditionally made tofu should be low FODMAP. Tempeh is low in FODMAPs too–this is likely due to the fermentation that occurs in its preparation–which reduces the FODMAPs in it.
Dyspepsia–everyone is a bit different. I would hope you are working with a dietitian that is well versed in digestive health. Likely you will need some additional diet modifications–but low FODMAP may make enough of a difference–and I wish you the best!!
Kate
Michelle
Hi Kate,
I find the hardest thing to stay away from is alcohol. If I am out with friends and want to drink what is the lowest food map alcohol? thanks!
katescarlata
Alcohol is a GI irritant–so fodmaps or not–should be enjoyed in moderation. That being said, a dry glass of white or red wine should be okay.
Laurinda
Regarding re-introducing high FODMAP foods after the elimination stage, and starting with Stage 1 (Mannitol) the recommendation is to try either cooked mushrooms or cauliflower. TWO QUESTIONS: 1. If I have no symptoms with say, the mushrooms, do I keep increasing the amount until I do experience symptoms; or, do I assume I’ll be OK with cauliflower as well (also Mannitol) and move onto Stage 2 (Sorbitol)? 2. Much later with the Fructose Stage, should I test for all foods there (mango, persimmon, watermelon, blackberries etc) and also in larger and larger amounts; OR does one start with a large amount (1 cup full), see the reaction and then reduce the amount?
Sources also vary in terms of the length of food challenging: some say 1 week and some 2 weeks; some say to try every 3rd day; others say for 3 consecutive days. Very confusing!!
katescarlata
Laurida,
It is confusing! And, just like there are different ways to wrap a present, there are different ways to approach food challenge. Not everyone does the challenges exactly the same. Some encourage a more aggressive challenge in an effort to try to evoke symptoms–so push larger quantities of a challenge food and some suggest a more gentle or cautious challenge. I like cautious challenges…so that is what I do in my practice. There are a couple rules with the re-challenge or re-introduction phase of the low FODMAP diet that you should be sure to follow: Make sure you stay on the low FODMAP during all the challenges and be sure the ‘test’ foods you use to test for each FODMAP group only has the FODMAP you are testing (not multiple FODMAPs)–so watermelon would never be a test food–during the initial challenges as it contains multiple fodmaps.
I have my clients start with 1/3 cup cauliflower on day 1 of mannitol challenge–if no symptoms they increase to 2/3 cup the next day. If they typically enjoy large servings of cauliflower they may increase to a cup of so and check their tolerance on day 3. If they pass cauliflower, they may decide to try mushrooms. With fructose challenge, I would start with half a mango day one–then day 2 increase to whole mango (if they normally eat a whole mango in a sitting-if they never would –then they may stay w/ 1/2 mango for 3 days….Anytime a person gets a reaction, the challenge would stop. Hope that helps a bit.
Ally
Hi Kate,
I would appreciate your advice regarding corn. Although the MONASH application indicates that a 1/2 cup serving of corn can be tolerated, there appears to be conflicting information regarding tortilla/nacho chips. Many of the food guides recommend corn and corn products; however, I believe I am having a reaction when I consume nacho chips (major bloating) and I am trying to narrow down what I can and cannot eat. Perhaps there is something that happens when the corn is processed, or there is a recommended serving size. Please let me know if you have any information or guidance on this.
It would also be helpful if you can recommend a dietician in the Toronto area (Canada). I am having difficulty trying to find someone using the published FODMAP resources. Many thanks for your help.
katescarlata
Ally–Here is a good review of corn products and FODMAP content that my colleague Patsy Catsos wrote: http://www.ibsfree.net/ibsfree_at_last/2013/10/why-is-corn-so-confusing.html
Sometimes it’s not the corn but other things in the corn products such as fat that can trigger symptoms so do keep that in mind. Or perhaps simply eating too much period. It’s hard to stop at a a couple handfuls of tortilla chips, right?! As for serving sizes on nacho chips–tolerance does vary person to person but I try to keep to the serving listed on the bag.
I would check out Stephanie Clairmont–she might be a good fit for you. http://stephanieclairmont.com
Ally
Thank you Kate – really appreciate the guidance. I will get in touch with Stephanie. I do tend to eat an entire plate of nachos. 🙂
Laurinda
Thank you, this was a huge help. With food challenging, is it safer to rather do every third day (because some reactions can take up to two days to manifest) in stead of 3 consecutive days? For how long should one challenge? One week? Ten days?
katescarlata
That is really up to you. Most FODMAP related reactions are likely to occur within 3 hours–but certainly in a constipated person may take a bit longer…and certainly some of my clients feel the reaction the next day. I typically recommend to challenging 3 days in a row-but if you prefer you could do every other day using the same challenge food over the course of a week.
Jena
Hi Kate,
Is Stevia low fodmap?
Thanks,
Jena
katescarlata
Stevia is low FODMAP–but read labels–some stevia products have other additives.
Laurinda
Hi Kate,
My first week of food challenge went well (Mannitol – I tested mushrooms) with no symptoms. Can I assume I’ll be symptom-free with ALL the foods in the Mannitol group, if I normally eat the amounts of foods stated in the FODMAPS app?
I read in the Food Intolerance Management Plan by Dr Sue Shepherd that one can follow any order of FODMAP testing that suits one: since it’s probably sensible to keep the GOS test for last, can I test Fructans before Fructose for instance? Do I then have to test the three stages of Fructans in 3 consecutive weeks (wheat bread; garlic or leek; cooked onion)?
Lastly, at what stage would I be able to bring back the following: fennel seeds; Oolong tea; dark chocolate; FOS prebiotics; cashew and pistachio nuts (the nuts after a successful Fructose test perhaps?)
katescarlata
Laurida- It a might be a good idea to try a couple different foods with excess mannitol to see your tolerance unless you would never eat them mushrooms and cauliflower together. Or you can move on…..and try that later. GOS foods are best tested last b/c most of them also contain some fructans as well as GOS. You don’t have to do all three fructan tests in a row. Most people fail onion so go easy on that one. After all of the individual group testing–you can then slowly venture trying foods w/ multiple FODMAPs–such as nuts, apple etc..But remember FODMAPs have a cumulative effect so try small portions of these foods that have multiple FODMAPs. So if you pass sorbitol and fructose–you might try a few apple slices on a salad. This is typically done w/ guidance of an RD that can individual your challenge phase based on your history and results w/ food challenges.
Danielle
Hi Kate! I’m loving your blog! It’s the most informative site I’ve found on FODMAP diet that I have seen 🙂 What do you think of coconut palm sugar and palm sugar? I know they are lower glycemic than table sugar and contain less fructose than table sugar but I also read that they are lower glycemic because they contain inulin. I had some gf cookies that contained palm sugar and got a very bad reaction…I’m assuming it was the inulin in the palm sugar. Funny thing is, coconut palm sugar seems to work ok with me, so maybe they contain different amounts? I would love to hear your opinion on these sugars because I have a cabinet full of coconut palm sugar and the liquid sap lol! Thanks, Kate! 🙂
katescarlata
Danielle, The Monash team tested palm sugar and gave it thumbs up (green light) for 1 Tablespoon portion. Not sure that coconut palm sugar has been tested. Anything with low GI makes me suspicious. So I say try to avoid on elimination phase of the diet–and maybe explore your tolerance with it when you are on the re-introduction/ challenge phase of the diet. It’s hard to know for sure–could be something else in the cookie you tried that bothered you and not the sugar at all. Don’t throw the cabinet full of sugars away yet…but you may want to hold off and test them carefully after the elimination part of the diet. And….thanks I am happy you are loving the blog…as I say over and over…it is a labor of love. Since I know personally what it’s like to have tummy trouble….I want to provide accurate info for those who struggle too.
Timothy
Hi Kate,
I’m starting a low FODMAPs elimination diet. I don’t have an RD in my town that is familiar with it, so I’m going to do my best with your info.
In your FODMAPs checklist it said instant coffee was high fodmaps, but espresso is low. What would filtered drip coffee fall under?
Thanks for the awesome resources!
katescarlata
Timothy–be sure you have the latest check list–Monash re-tested their coffee and cocoa-so I have updated my list. I believe filtered coffee would be similar to expresso–just keep to 1-2 cups and remember caffeine can be a GI stimulant and irritant.
Timothy
Thanks Kate. You’re right about coffee. I’ve decided that if I don’t get relief from a low FODMAPs diet in a few weeks, I’ll do an elimination diet with coffee to be sure. This is going to be a good year, IBS is goin’ down! 🙂
Samantha Matete
Hi Kate, is cassava flour gluten free and low fodmap???
Well Balanced - Food - Life - Travel
Not sure about cassava flour. Have not seen any data. But it is gluten free. It’s from a root not a grain.
Jackie
Where would I find good in depth information of collagenous colitis and IBS. Where would I go to get a breath test. Your blog is wonderful, very up-to-date and informative. Thank you for all your time and energy.
Well Balanced - Food - Life - Travel
Jackie, breath tests are generally done at a big hospital –in the gastroenterology department. But, there are also home kits that you can investigate. This lab is reputable: http://hydrogenbreathtesting.com but typically a doctor will order the kit for you–and help you review the results and prescribe antibiotics if indicated. Here is some info on collagenous colitis with other resources you may find helpful at the end of the page. http://digestive.niddk.nih.gov/ddiseases/pubs/microcolitis/
Jeanne Burt
I have a 19 yr old daughter with IBS and chronic fatigue serious enough to have her out of university for this year. All blood/urine testing negative, including for bacteria, celiac, fructose–no pathology at all. She had blood testing for food sensitivities (200 foods) and numbers were high for dairy (which she already knew), gluten, soy, 4 kinds of nuts, egg whites, white potatoes, celery, radishes, yeast and many more. I have taken all of these foods out of her diet and the diarrhea/bloating/cramping have lessened but she has reached a plateau. I am now going to try to eliminate the FODMAPS foods as well. She’s left with a very restricted range.
l. What is your opinion of food sensitivity testing? The gastroenterologist and food allergist don’t give it much credence. But it has been the only life raft we’ve found so far in the IBS ocean.
2. Does it make any difference to FODMAPS levels if foods are cooked vs raw? Cooked onions and garlic and apples don’t seem to bother her at all. Or am I fooling myself?
3. We live in Ottawa, Ontario. Is there a RD or nutritionist here you would recommend? I’ve been all over the net and even our gastroenterologist doesn’t know anyone with an IBS/FODMAPS focus. She has seen a nutritionist who was very vague in her recommendations and a naturopath who has helped some. So you ever come to Ottawa?
Been at this about 5 months now and so, so tired and overwhelmed. I’m sure I’ve made lots of mistakes in handling the whole thing but mainstream medicine has really left us on our own. Nobody should be tired, ill, housebound and afraid at 19. Dear Ms Scarlatta, please talk to me like the novice that I am–the science involved in FODMAPS is too complicated for me to follow (i.e. fructans/fructose/GOS/order of testing etc.) so where to begin? All advice will be most appreciated.
Apologies, I was going to try to be brief.
Well Balanced - Food - Life - Travel
Jeanne–try Stephanie Clairmont: http://stephanieclairmont.com/contact/ Not sure how close she is to you but she does phone consults. In some cases, cooking FODMAP rich foods could alter their content if you were cooking in water and draining off the water. Some of the water soluble fibers could leach into the water and be drained off. But for the most part–not sure this would make a BIG difference for most fodmaps in foods. Sounds like you need someone to help sort out all the details and unfortunately it would not be advisable for me to do this in a blog format. I would need a full history and much more time to comb through your daughter’s medical history. I hope that Stephanie might be a good resource for you. Consider evaluation for small intestinal bacterial overgrowth if this has not been tested.
Sheryl Lawrence
Hello Kate,
Could you weigh in on taking enzymes while on the FODMAPS diet? My integrative med doctor recommended them (they do contain plant cellulose, maltodextrin and “soy(trace)”, free of sugar,wheat,casein, gluten,milk, yeast, gelatin,peanuts, tree nuts.
Thanks so much for all your important information.
Well Balanced - Food - Life - Travel
Sheryl, I don’t typically need to recommend digestive enzymes for my clients on a low FODMAP diet BUT occasionally some of my clients do need them due to ongoing malabsorption– the cellulose, maltodextrin and trace of soy should be okay from FODMAP stand point.
Sheryl Lawrence
Thank you for such a prompt response! One more quick question: I believe from my ongoing symptoms, many autoimmune conditions,years of inconclusive tests by doctors who don’t believe diet can be a cause, a SIBO breath test would be greatly helpful. (I’ve been in the care of Dr. Mark Heyman in Lenox, Mass and his nutritionist agreed with me trying FODMAPS and recommended your blog.) Can I request this test without a gastroenterologist insisting that I go through a whole battery of other tests first? I did have an endoscopy, blood work, cultures taken years ago with no positive results of anything and just the recommendation of taking Culturelle which of course, did nothing. Is asking for a SIBO breath test a red flag for a doctor who will think I am just self-diagnosing?
Your advice and knowledge is so appreciated.
Thanks,
Sheryl
Well Balanced - Food - Life - Travel
Sheryl, I believe any patient diagnosed with IBS should undergo a breath test for SIBO. The test unfortunately is not a validated test and has limitations–but at present it’s the best we have. Your PCP can refer your for testing. The breath test is simply one test to determine whether you have bacterial overgrowth in your small intestine. If you do have bacterial overgrowth–then next step outside of treatment (antibiotics/diet change)–is to work with your gastroenterologist to try to determine the reason you may have developed the condition–do you have another autoimmune disease that is increasing your risk for SIBO, do you have a significant motility disorders that may benefit from medication, do you have pancreatic insufficiency, adhesions, etc. I would not say that you are self-diagnosing but rather advocating for your health! Big difference!
Antonia Pogue
I’ve been getting a lot of conflicting information on celery and pumpkin. Are these ingredients low FODMAP foods or not? I would like to use canned pumpkin for baked goods. I see celery all the time in low FODMAP recipes.
Thanks for any help.
Well Balanced - Food - Life - Travel
Antonia, celery should be okay in very small quantity–<1/4 of a large stalk BUT not huge quantities. It does have some mannitol. The issue around pumpkin is US canned pumpkin is different from what Australians term pumpkin. Australians call squash pumpkin. I have sent the Monash researchers US canned pumpkin for analysis and should have a better understanding of whether its suitable on the low FODMAP diet or not very soon!
Ashley Chase
are there recommended cough drops I can use? – I just started the elmination phase and of course woke up with a huge sore throat
Adrienne Groh
Just came across your site…very helpful. Diet is working well. Unearthing triggers. I am very lactose intolerant so am making my own kefir. It’s delicious. I put a very small amount of concentrated cherry extract in it. Easy to make with yogourmet freeze dried kefir starter(yogourmet.com). My house is drafty so I make it in a quart canning jar wrapped in a dishtowel and leave it by a small room radiator for 24 hours…voila, no lactose. Make it with whole milk for great texture. I’ve heard one can put it in a cold oven with the interior light turned on…but for 24 hours.
Meech
I just noticed my toothpaste has mannitol in it. Can this affect me, and has anyone found a brand that has no high foodmap ingredients but still works? Ive tried all natural toothpastes but they made my teeth look less white.
Heather
I’m confused about spelt – Monash says yes to sourdough spelt bread, but doesn’t mention spelt flour or intact spelt grains. Does the sourdough process affect the fodmap content?
Well Balanced - Food - Life - Travel
Heather–spelt is a grey area. Growing conditions can effect FODMAPs so we need to check spelt grown in various places in the world. I think its worth a try–but perhaps best during the re-challenge phase. Sourdough breads tend to have less FODMAPs–at least less fructans. We have sent various US breads for testing…so more to come.
Erin
Kate, Can you tell me if hazelnut, walnut and pecan flour are okay during the elimination phase of the diet? Also, what about seasoned,Nori? It is roasted with oil and lightly salted. I also found a soda at Whole Foods made with sugar instead of HFCS. Would that be okay to drink occasionally? Thank you,
Erin
Kate, Can you tell me if walnut, pecan and hazelnut flours are okay during the elimination phase of the diet? What about seaweed, nori? It is roasted with oil and small amount of salt. I also found a soda made with sugar instead of HFCS at Whole Foods. Would this be allowed on an occasional basis?
Thanks,
Erin
Sorry, I didn’t mean to post my comment twice. There was an error when I submitted the first post. So, I didn’t think it went through.
Well Balanced - Food - Life - Travel
Erin–hazelnut is the highest in FODMAPs and probably would only be able to use 1-2 Tablespoons before being a FODMAP cut off. Walnut and pecan only slightly more. So…the answer is –if you are using small amounts to add to a recipe and you would not consume more than 2 TB you may be okay–otherwise–wouldn’t use on elimination phase. Nori is okay per Monash app. Soda sweetened with sugar would be okay–would limit to 1 cup and use as a treat. As sugar offers little health benefit as you know. 🙂
Sally
Hi Kate
I have been following the fodmap diet for a week and for the first 4 days felt great … Now however bloated and constipated … Any advice?
Well Balanced - Food - Life - Travel
I can’t really recommend specific guidelines in a blog format as I don’t have your medical history. What I can share is that many people drop their fiber intake too low on the low FODMAP diet and need to be sure that their fiber and fluid intake is adequate. Chia seeds are a great high fiber and low FODMAP option that many individuals can tolerate. Adding a tablespoon of oat bran to hot cereal can be helpful as well. One of the way FODMAPs can be troublesome is that they draw water into the intestine. So on a low FODMAP diet –this can lead to less fluid in the colon and for some people this can be an additional contributor to constipation. One of the keys to a happy intestine is being ‘regular’. Here is some additional info on FIBER content of low FODMAP foods: https://blog.katescarlata.com/fodmaps-basics/fiber-without-fodmaps/
Carolyn
Hi Kate, I’m happily following a Fodmap diet. Have two queries. First is it ok to eat coconut flesh or drink coconut milk? Secondly I love Asian field green vegetables eg morning glory. Is this ok? Thanks for a wonderful blog.
Carolyn harmer
Chloe
Your thoughts on Calcium Caseinates? Ok or not?
Well Balanced - Food - Life - Travel
Chloe, From what I have read–calcium caseinates should be okay. It it possible for trace amounts of lactose to be found in them–but probably low amounts.
Karen Olson
I am going to ask my PC for a referral to meet with you. But while I wait for that process to play out I am starting to follow the FODMAP plan. I am in a bad flare of IBS and have fibromyalgia and Sjogrens as well. Any encouragement that FODMAP will address these issues? I am a working girl and love my job, but am having a very difficult time keeping up lately. I am looking for nutrition to support as normal an active life and schedule as possible. Thank you, I looks forward to meeting with you.
Well Balanced - Food - Life - Travel
Karen, I would suggest you get tested for small intestinal bacterial overgrowth–if you have not been tested yet. I have found that some of my clients do note improvement with fibromyalgia symptoms w/ low FODMAP diet and bacterial overgrowth treatment, if present. I look forward to meeting you!! I will try my best to help you manage your current symptoms.
Timothy
Kate,
I need to ask a question and I’m sorry if it’s tmi, but I really need to know if a FODMAP diet may help.
I frequently see undigested food from my bms, lots of bits on tissue. Also terrible gas and bloating (mostly at night). I have a hard time gaining weight also. Have you heard stories like that from other patients and does the low fodmap diet help?
Do you do any diet consultation via Skype or email? There are not any dietians in my town familiar with FODMAPs or SIBO.
Thanks.
Meech
I am sending out a plea to other fodmappers to start writing to health food companies and stores to request they look into the fodmap certification program. it would be amazing to start seeing some fodmap friendly certification stamps on food products, like there is for gluten free or non-GMO products.
Us fodmappers are going to have to raise awareness of this diet to health food companies and stores so that they become aware of the market for fodmap friendly products. Lets flood the health food comanies with these requests and maybe we can start seeing the fodmap friendly certifications in our grocery stores!
The website for the certification program is fodmap.com if you want to check it out. (I have no affiliation with the program, I just want to make grocery shopping easier for all of us!)
Jennifer Page
Hi Kate! I have read your Eating Well With IBS book and have a question about some of the recipes. I see the recipe for BBQ pork-but I thought BBQ sauce wasn’t ok for those with Fructose Mal. Is this correct? Also, is paprika an ok spice to use? Monash app doesn’t list it, but another FM app I have says it is not. Thank you!
Well Balanced - Food - Life - Travel
Hi Jennifer–MY Eating Well with IBS was published 4 years ago–and I wrote it 5 years ago…so the info is quite antiquated. It is still a good introduction to understanding IBS and the various triggers–but not up to date on FODMAPs. The low FODMAP is evolving monthly—with new research– so best to get books with this years publication! I keep my FODMAP checklist up to date on this blog. Paprika has not been tested as far as I know…but I don’t suspect it will be an issue. And you are correct–most BBQ sauces have tomato paste, molasses or HFCS so would not be suitable on the low FODMAP diet. You can always sub in my BBQ recipe https://blog.katescarlata.com/2012/10/11/homemade-bbq-sauce-fodmap-friendly/
Amber
Kate – first and foremost, thank you for the incredible resource that you provide. Your site, Monash, and a handful of books have been a lifesaver these past few weeks as I’ve tried to get my years-long symptoms under control. Any personal recommendations for an expert FOD MAP clinician around the Rochester, New York area?
Well Balanced - Food - Life - Travel
You are most welcome Amber. I do not know of an RD in the Rochester, NY area. Some near Albany –but I realize that is quite far away!
Beth
Amber,
I just found this and was wondering if you ever found anyone in the Rochester area?
Jennifer Page
Thank you! I look forward to trying your BBQ sauce, it sounds yummy! 🙂
Pone
Have you heard of any problems for celiacs or FODMAP sufferers using the sugar alcohol erythritol? I thought I had found the perfect sugar substitute but I am starting to suspect I am having a severe metabolism issue with it.
Well Balanced - Food - Life - Travel
YES, I have heard about this. Two potential problems occur 1) Erythritol is supposed to be a well absorbed sugar alcohol BUT….it has been shown when used in combination w/ fructose –it contributes to GI symptoms. 2) Sugar alcohols are absorbed via pores in sm intestine… “pore size is affected by mucosal disease; pore size reduces in celiac disease where erythritol is poorly absorbed.” Noted in this article: http://www.medscape.com/viewarticle/716634_6
pone
The Medscape link you provide requires a login. Do you have a link to the full text of study or at least a good abstract? What is full title, author, and date?
I have never had any GI symptoms with erythritol. In fact, from that point of view it has been a perfect sugar substitute. But I am having some kind of neurologic effect from some food I am eating. Just the vague feeling an hour after eating that there is *something* in your system that makes your brain weak, unfocused, distracted….
I used to get this in a very extreme form with wheat but wheat has been out of diet for years. Three months ago I also took out potential cross reactors like rice and dairy.
It’s very difficult when you have so many foods that your body wants to treat as invaders, that stimulate immune responses. I am so tired of food being the enemy, of having neurotoxins in me in spite of being so careful with diet.
Well Balanced - Food - Life - Travel
Anyone can sign up for medscape. I would encourage you to do so–then you can access all sorts of free articles.
You may benefit from working with an integrative MD that can look for other pathways that may be compromised that are contributing to your brain fog. Inadequate zinc and subsequent chloral hydrate production can contribute to brain fog. Glutathoine production helps detoxification–perhaps you need supplements to help support this pathway. Working with an MD that can evaluate what might be additional contributors to your ongoing symptoms is essential. You don’t want to randomly remove dietary components that help fuel and restore your gut. Adequate nutrition is key to rebuilding and renewing your intestinal lining.
pone
I looked unsuccessfully for an “integrative MD” for years. I tried to get an appointment with Chris Kresser, but his back office is a nightmare. They dropped me from a waiting list after I was on it for years, then added me and dropped me again because I didn’t reply to one email. I lost years because of this.
I find that the vast majority of integrative MDs who run blogs or web sites want to get speaking engagements and write books, not see patients.
You find a lot of people who are chiropractors who put their shingle for integrative medicine, but most of those do not look well qualified to catch things that are truly medical, not nutritional. The “Paleo MD” directories I have seen are loaded with these types.
At this point I have scheduled visits with specialists and will integrate in some work with nutritionists as well.
Anna Gerrish
Hi Kate! I just stumbled on your website today and I’m very excited about all the information you provide. Four years ago, I started having problems with IBS-C, but it got out of control about 2 months ago. I’m now 85 pounds and trying to deal with my fear of food in general, because I’m afraid that what goes in won’t come out. But I’m trying to find ways to add good fat and calories and thought about peanut butter or sun butter. I’ve read conflicting reviews on whether or not they cause constipation, so I’m wondering what you think about them? It would be wonderful if they were ok!
Well Balanced - Food - Life - Travel
I like the peanut butter best–all natural. The sun butter is an option–but sunflower seeds have more FODMAPs–so just 2 teaspoons per sitting is appropriate. And of course a drizzle of olive oil is always good–add to vegetables, grits, GF pasta to boost healthy fat calories. I hope you get some assistance to boost your calories and nutrition. Consider a therapist or perhaps hynotherapy to help with fear of food. (which is quite common by the way–when eating hurts–its easy to fear food….but unfortunately you need good nutrition to help your gut heal).
Dawn
Is custard ok if it is made with Lactose free milk from powder?
Well Balanced - Food - Life - Travel
Would think so. But haven’t seen lactose free powdered milk…
Dawn
Custard powder, lactose free milk
Well Balanced - Food - Life - Travel
Custard powder is a new one for me. It is not too popular in American cooking. If it’s made with corn starch and vanilla that should be suitable.
Rachel H
Hi Kate,
Thank you so much for this blog-it is incredibly helpful! I live in Ireland so the resources are fairly limited for this diet. I just have a quick question- what is the FODMAP rating of vegetable stock cubes? I usually use a yeast-free veg stock cube to make soups but I’m unsure whether that will work with the low FODMAP plan.
Thanks in advance!
Well Balanced - Food - Life - Travel
Not sure–but I haven’t found one that is suitable. Feel free to send list of ingredients and I can do my best to help you. Typically these products have onion and/or garlic. This might show up on a food label stated as ‘natural flavoring’.
Snenny
Hi Kate,
Apple and applesauce are obviously not on the fodmap friendly list, but I was wondering whether it would be ok to use 1/4 cup apple sauce making muffins (so it would be divided between 12)? I often use apple sauce to replace some of the oil/butter.
Thanks for your help and advice 🙂 and for your website! It really has been a godsend on the low fodmap diet!
Snenny
katescarlata
Thanks Snenny. I wouldn’t use the applesauce. You could try to add some banana to sub out some of the oil.
Becca
Hi Kate,
I think I asked this somewhere, but I forgot to tag it so I could re-find it…Are anchovies low FODMAP?
Thanks so much!
Mary
Hi Kate,
Why does the low fodmap diet limit nuts and nut butter to 2 TBS per day?
Since being on a paleo diet I am finding I am sensitive to almonds now so I am avoiding them for awhile anyway.
Since fructans are water soluable does that mean that if I find I can tolerate small amounts of broccoli then I should sauté it in oil instead of cooking it in water?
Thanks!
Mary
katescarlata
Mary–Nuts contain fructans and GOS–so limits are set to keep your intake under the FODMAP cut off. Cooking broccoli in water theoretically would be the best method to decrease the fructan content. We cook garlic in oil as we don’t want the waters-soluble fiber to leach in the oil (then of course remove the garlic but enjoy the garlic infused oil) So…the opposite is true when we want to reduce fructans–cook in water–let the fructans leach into the water–then toss the water along w/ the fructans. HOWEVER–I have not seen actually data on this cooking method and how much fructans are removed. Hope that provides some clarification.
Jennifer Page
Hi Kate-My 16 year old son has Fructose Mal. and we are following the FODMAP diet. He recently had a touch of a stomach bug and we are having trouble regulating his system. Lots more gurgles and pain than a week prior. I am not sure what to do/take out of his diet/give him to help. His GI dr has very little knowledge of FM or SIBO and isn’t very helpful. Do you have any ideas or suggestions in his diet to help calm his system down? Thanks, Jen
Megan
Can you tell me how many grams of sugar a day is okay on a FODMAP diet?
Thanks!
Wendau
This is the best website I’ve seen on the subject – thanks so much!
Since I love broccoli, avocados and tomatoes, I was wondering if I could still eat them if I take digestive enzymes before or after eating them?
Also, I just bought a natural jam with “apple pectin” listed last (hard to avoid that ingredient). Is that ok if I only have 1 tablespoon?
Lastly, I’m not clear on the excess fructose component – why is fructose is in excess of glucose an issue, rather than just the amount of fructose or glucose?
Thanks!
katescarlata
Broccoli (1/2 cup). 1/8 avocado and fresh tomatoes are allowed on the low FODMAP diet. Just try to spread them out over your meals to enjoy your favorite foods—but take care of portion size as the amounts I listed are the amounts allowed on the low FODMAP diet.
Apple pectin is not a FODMAP source as far as we know==but rather a polysaccharide (a longer chain sugar). BUT–it is a rapidly fermentable sugar so may trigger symptoms. And regarding your fructose/glucose question. Glucose is the helper in fructose absorption–so when there is glucose present–fructose is better absorbed.
Elaine Rey
Any word yet on nutritional yeast? It adds such a nice cheesy flavor that I am hoping it is okay. And it is ALL mushrooms that have polyols. Even my beloved shiitakes?
katescarlata
Not sure that all mushrooms have been tested–but certainly, try out others to see how you feel. Think nutritional yeast would be okay–but I have not seen data on it.
Alice
Are glucojels jelly beans low fodmap? they contain: sugar, glucose (20%), starch, flavour, food acid (citric acid) and colours. Also what about quest bars and carob chocolate?
Thanks
katescarlata
Alice–based on what you listed the jelly beans in reasonable portion look okay. Carob is high in oligosaccharides–so not allowed. Not sure about quest bars. Feel free to send list of ingredients and I can give you my best guess.
M-A
Hi Kate, I think I may have found ready-made cookies that are low-FODMAP, but some of the ingredients listed I am not sure about and I was wondering if you could help me? The ingredients in questions are: tapioca flour, potato starch, amaranth flour, kale powder, tapioca syrup, organic palm oil, coconut oil, palm sugar…Many thanks!
katescarlata
Aimee–not sure about the amaranth flour or kale flour. Puffed amaranth has a 1/4 cup limit and kale and kale flour may be very different in regard to FODMAPs. Otherwise–my guess is the other ingredients should be okay. I might test my tolerance with one and see how I do.
Eileen
Do you have any FODMAP friendly picks from the Jamba Juice menu?
katescarlata
Eileen…I think those types of fruit-y drinks have too much fruit in them to suit the low FODMAP diet -or add milk upping the lactose content. You want to stick w/ one serving of fruit at a sitting during the low FODMAP diet and many fruit drinks you get out in those large cups have far more than 1 fruit.
Megan
I’m wondering which baking extracts are safe on low FODMAPS….I know vanilla extract is okay, but I can’t find any information on others. Is the extract “safe” as long as the food is too?
crabby
What a great resource, thank you!
I’ve had constant uncomfortable bloating for years, and finally saw a GI doc who doesn’t think it’s IBS (not much of any bowel symptoms), and am awaiting some blood work. But he suggested a low FODMAP diet. And when my situation is clearer I want to scout out a dietician to guide me. (Happen to know anyone Cape Codish?)
But in the meantime, I’m trying to reduce fodmaps generally and track particular foods & bloating to figure out MY prime suspects. The problem is, I don’t know how long it typically takes a food to cause bloating.
If I find myself blowing up, I don’t know if it’s the food I just ate, or whether it could something from a previous meal. Sometimes it seems I start bloating almost immediately after eating, but would that make sense given the transit time food would need to cause trouble? Or can it be fairly immediate? But then there seems to be gradual expansion as well over the course of a day. If you have an old blog post on this you could refer me to, I don’t want to take up your time re-answering, but if not and you happen to have some info on this, would love to hear your take.
And it’s so impressive you actually come back and answer people’s questions given how valuable your time is! Again, very much appreciated.
katescarlata
I would recommend Nicole Cormier–she is practicing on the cape 🙂 http://www.deliciouslivingnutrition.com Bloating can occur for many reasons. Some patients find just thinking about food or drinking water exacerbates their symptoms. Your intestine can get moving in anticipation of eating. Salivating at the thought of a good meal or something you like can start just because your brain is letting your GI tract know–something yummy is on its way…this can trigger GI movement. If you have gas in your intestine–and it moves to another place while you start eating–this can feel immediate. I would strongly recommend you get tested for small intestinal bacterial overgrowth. Classic symptoms are a build up of gas as the day goes on–presenting as ‘gradual expansion’ over the day. For some people, food leaves the stomach in 15-20 minutes and if there are bacteria waiting in the beginning part of the small intestine–they will start fermenting the food and create gas. So, the answer is–bloating can start at any point–most often when the food travels to the colon–but in small intestinal bacterial overgrowth this can happen sooner. I would also recommend you have some motility testing if you haven’t to see how your stomach empties and how fast or slow your small intestine moves.
crabby
THANK YOU!!
This was extremely helpful! (I am an enthusiastic envisioner of upcoming meals, so it’s funny to think my anticipation could be contributing to the problem!) And I really appreciate the dietician recommendation; she looks great and I definitely need some guidance. I think SIBO may be on my GI’s radar, though I don’t know how he feels about ordering testing, as I gather not every doc is a believer. But it does sound like a real possibility from what you describe. I’ll ask him about it after the bloodwork’s done.
Again, the info and help you provide here is amazing and much appreciated!
Megan Tavares
my doctor as put me on this low FODMAP diet and under grains/breads it says on my sheet to avoid wheat. also it says to avoid lactose, and also says not to eat soybeans. so does that mean i have to be lactose free, gluten free, and soy free. im really confused.
katescarlata
Hi Megan, First of all…please don’t try to do the low FODMAP diet on your own. Get help from a dietitian knowledgeable in digestive health and the diet specifics–it will make it a whole lot more easy and enjoyable–probably tastier too! But, I will try, in brief, to give you a few tips to head you in the right direction! The low FODMAP minimizes small chain carbohydrates. Gluten is a protein–found in wheat, barley and rye–(these grains also contain FODMAP carbohydrates known as fructans and GOS). So although gluten is not the focus of the low FODMAP diet—it is reduced on the low FODMAP diet as wheat, barley and rye, (the primary gluten sources in the diet) are minimized on the diet due to their FODMAP content. Soybeans–in their whole state–the whole bean, are a source of GOS, a FODMAP. Soy protein isolate–however is not a source of FODMAPs (protein is not a carb!) It is the carbohydrate/fiber part of soybean that contains FODMAPs. So…it’s not a blanket statement–avoid all soy on the low FODMAP diet–as the low FODMAP diet is specifically reducing the carbohydrate part of soy only! The low FODMAP diet is low lactose or lactose free—but it is not dairy free. You can eat low lactose dairy foods such as aged and hard cheeses. Hope that helps!
Megan Tavares
Thank you Kate i am not seeing my nutritionist until September unfortunately, so at the moment i have to figure it out on my own. Which it is a nightmare going grocery shopping. This did help a lot. What ive been doing so far is been buying gluten free products to avoid wheat as much as i can and trying to stay away from milk products. However sometimes the product contains “MILK, or SOY”.. for example “i cannot believe its not butter” has soybean oil, sweet cream buttermilk, and soy lecithin.. so is something like that be okay to have? Because is that soy stuff a carb or protein..i have no idea. Also i know i can have gluten free bread because it has the soy protein so now that clear to me. It said i could have potato bread but the ingredients has unbleached enriched wheat flour, nonfat milk, wheat gluten, soybean oil, butter, cream yeast. so is that okay also.. i was confused because it said i can have potato bread but yet it said it has “wheat gluten” in it.. im sorry i just am confused with the milk and soy because if its not in one thing its in an another. if you could give me answers to these two examples i provided it will help even alot more.
Megan Tavares
Would it also be easier to check the nutrition labels and see what it says for total carbohydrates?
katescarlata
Total carbs on a food label can refer to low FODMAP carbs too–so this would not be the direction I would go–you would likely limit things you don’t need to.
Why not just start with my grocery list and checklist –and create a few meals from those resources. Ease in –rather than trying to read unlimited food labels which can be overwhelming even for a dietitian!
Soy in an ingredient list is low FODMAP when it’s soy protein isolate, soy lecithin, soy oil–soy is a potential FODMAP source when listed as whole soy bean or soy flour, –which would contain the whole soybean. Milk in a product could be a FODMAP source. This would be an example where you could look on a nutrition label and check for sugars. Lactose is a sugar–so if the product is cheese or butter/margarine –look at sugar content. If it is 1 or less–this product is very low lactose and should be tolerated on the low FODMAP diet–from the lactose vantage point.
alexis
hey im on the 3rd week of my diet i added dairy back in for 3days can i continue to keep the dairy in my diet if it has not caused irritation?
Janet
I was wondering about Tofutti “Better Than Sour Cream” sour cream–is it fodmap friendly? I am trying to find something that I can use as a base for dip.
katescarlata
Janet–I am not loving that the second ingredient is partially hydrogenated fat–but it appears to be fairly low FODMAP from my perspective.
Em
Hi Kate, I’m confused about corn! It appears from the Monash University app that cornflakes contain moderate amounts of oligos fructose and portions need to be reduced. Yet gluten-free cornflakes are shown as low fodmap. How can this be as gluten is not part of the fodmap picture? Also are taco shells (made with cornflour) ok, and what about tortilla chips? Thank you for all your advice
Cecilia
Kate: very useful website and bog! How can I gain more weight with a low FODMAPS diet? My weight has been sliding and this is not good as I’m already skinny!
katescarlata
Cecilia, I hope you are working with a dietitian to help provide a plan with adequate calories. Including a balanced menu every time you eat is one way to boost calories. Have you seen this handout? https://blog.katescarlata.com/wp-content/uploads/2014/07/How-to-make-a-low-FODMAP-meal-final-pdf.pdf
Cecilia
Kate:
Thanks for this for this FODMAPS meal suggestion. I haven’t consulted an RD yet because I want my gastrointestinal specialist to diagnose that I, indeed, have this condition first. So, in the meantime, I’ll follow your meal suggestions.
By the way, I’ve been on HRT for over five years. Would that lead to my FODMAPS condition?
Cecilia
Ilaria
Why is it that some sites say ‘avoid cherry tomatoes’ and on other sites they’re listed as safe in a low fodmap diet and are used in several low fodmap recipes found online? Same goes for cabbage…some sites list it as high fodmap, whilst others say that common cabbage is safe…Also with regards cocoa powder, it’s listed as high fodmap, yet you’ll find unsweetened cocoa powder listed as ingredient in low fodmap recipe. Should goat cheese be avoided in low fodmap diet or is it safe? In the following link it says …”Some cheeses are not aged, including mozzarella, chèvre (goat cheese), cream cheese, marscapone, American, cottage cheese, ricotta, queso fresco, and feta. These can have more lactose, depending upon how much whey remains in the cheese.” (http://www.ibsfree.net/news/2014/6/8/cheese-and-fodmaps) so are mozzarella and feta safe as listed in other sites or not since in this site they’re listed along with mascarpone and ricotta which are high fodmaps. Dilemma with cream cheese too, as in some sites it says it’s safe, whilst in others it’s high FODMAP. Coming across contradicting information is so confusing.
katescarlata
I so appreciate your frustration and your are not alone. There are many conflicting lists of low and high FODMAP foods online. This is partly due to the fact the new food analysis has shown different info from the antiquated info researchers originally had access to when originally listing FODMAP food lists and also due to the way the health practitioner wants to apply this knowledge in their educational materials. Monash University has an app that is available for iPad, iPhone and android smart phones. This app provides the most up to date info–and also the amount of the food that is deemed safe by the researchers. To me, it’s worth it’s weight in gold! And supports funding for more food analysis! Info on app here: http://med.monash.edu.au/cecs/gastro/fodmap/iphone-app.html
Common cabbage in a 1 cup serving is considered low FODMAP in the app. 4 cherry tomatoes are low FODMAP too. Cocoa powder in small doses makes the FODMAP cut-off too–so about 1 US TB would be suitable (2 heaping tsp) I allow goat cheese, American, feta–in small amount–they don’t contain much lactose and as long as you limit to one serving should be suitable for most people. Most cream cheese (whipped is typically best) is fairly low lactose in small portion (PORTION Size matters!!)–2 US tablespoons of whipped cream cheese has <1 gram of lactose. If you ate 1/2 cup of it–the lactose might add up though! To help navigate these nuances–working with a dietitian knowledgeable in FODMAPs makes application of the diet a whole lot easier!
Cecilia
Kate:
Does this app work on iPads as well?
Cecilia
Kate:
Can I drink coconut water as part of the low FODMAPS diet?
Cecilia
Kate:
Can I drink coconut water as part of the low FODMAPS diet?
katescarlata
Small amounts of coconut water are okay–about 3 ounces. But more than that you will be ingesting too much sorbitol and frutans.
Cecilia
Thank you!
Jennifer Page
Hi Kate-In one of your email tips you stated that the low FODMAP diet is supposed to be temporary. Does that apply to those diagnosed with Fructose Malabsorption too? Just wondering…thank you!
Jen
Marsha Carroll
I am wondering if anyone who is following the LOW FODMAP diet has had trouble with Lactaid 2% milk.
Thank you!
Marsha
Elizabet
Oh Kate you’re a godsend! Thank you for all the information you provide here. I’m so happy to hear about the coconut milk, and for the quick reply! I hated to loose my coconut milk, after loosing so many other food treasures. I had a reaction to something today and I can’t quite pinpoint what it was but I did consume more coconut milk than normal (in 2-3 tbl increments). Now I can narrow it down to one of the other two suspects. Thanks again!
katescarlata
Elizabeth- coconut milk has a fair amount of fat too….so although not a FODMAP source —fat can contribute to symptoms in some.
Sometimes there are issues beyond FODMAPs.
Jennifer Page
Kate-What about flax milk?
katescarlata
Flax milk has not been tested as far as I know.
Thyra
Hi Kate
What a good blog you have 🙂
I was wondering about locust bean gum (LBG, also known as carob gum, carob bean gum, carobin, E410). I see you have updated carob as high fodmap, but do you know if LBG, which is made from the seeds is high in fodmap too, when used as a gelling agent?
Thyra
Oh, and do you also know which of the fodmap groups carob contains?
katescarlata
Carob contains fructants –small amounts 1 teaspoon would be allowed per the Monash University app…but more than that is over the fructan threshold.
Mary
Hi Kate,
Do you have any info on winter squash? I have the Monash app but they have not refreshed it to add new foods in a long time and there is very little information on it with regard to winter squash. Since the season is upon us and there is so much yummy squash at the farmers market I’m trying to determine which ones are low FODMAP.
Thanks!
Mary
Elizabet
Thanks for this question! I’ve been wondering too!
Kerri
Hi Kate – thanks for such a great blog! I’ve been following a low FODMAP diet for two years now but I’m seeing more and more information that suggests it should not be a long term solution. Is this correct? I still have many ‘bad’ days with my IBS even when I eat low FODMAPs.
katescarlata
Hi Kerri–that is true–it’s best to try to reintroduce foods back in –as you may find you are not intolerant to all FODMAPs. If you don’t experience adequate symptom relief w/ the diet–I would work with a dietitian to explore other reasons for your bad days. It’s fairly common for people to have more than just a FODMAP issue. You might need a better bowel regimen to keep your regular, you may have delayed or rapid emptying of your stomach contributing to other symptoms—work closely with your GI doc and dietitian to explore other ways to help you!!
Linda
I have been drinking Twinings Lemon & Ginger tea but have noticed that one of the ingredients is Blackberry leaves. I am only just starting a low FODMAP diet but am aware that Blackberries are on the High FODMAP list. Do you think that the Blackberry leaves could present a problem?
katescarlata
Hi Linda –the blackberry leaves have not been tested for FODMAPs as far as I know…and the leaves and fruit would likely yield different results–so can’t say for sure that blackberry leaves would contain FODMAPs. That would be a tea I might experiment and assess symptoms to after the elimination phase–since we just don’t know.
Mirte Kaan
Dear Kate,
I may have missed a message that already gives the answer, but there are so many on this page/already searched on your website but I couldn’t find it! I was wondering about Coconut Sugar? Is this Fodmap proof? I remember you had a blog about sweetners/sugars but I may be wrong!
Kinds Regards, Mirte
katescarlata
Mirte, coconut sugar has not been tested as far as I know. Palm sugar has been tested and small amounts (1 TB) are low FODMAP. Be careful when the food has a low glycemic index claim–especially sweet foods–this often means that the food is slow to digest or even malabsorbed so may lead to gas/bloating.
Carla
Hi Katie, We raise our own chickens and then make home made stock from the carcasses. I put carrots and onions in the stock. Is this ok? I don’t “eat” the onions, but could the stock be problematic since it is made with onions? Thank you….
katescarlata
Hi Carla, to keep the broth low FODMAP–you should not add onions directly to the broth. You could season some oil with onion, remove the onions, and add the onion flavored oil to the chicken broth. The onions have fructans, which are water soluble fibers. So if you add them to the water w/ the chicken in making the broth–the fructans can leach into the water. The fructans won’t leach into the oil–but will add some nice onion flavor to the oil–which you can add to the broth.
Carla
Thank you Kate for the advice on the broth. I have a lot in the basement, guess I will make new!! we pressure can the broth when done, would that have any affect on the fructan from the onion? I can do without the onion, just wondering if I can still drink what I have in basement. I am doing the FODMAP diet for GP, so not quite the issue as someone with IBS. Thank you!!
Goose
Hi Kate. Is Tequila a high fodmap drink/food? Thanks.
katescarlata
I haven’t seen actual data on tequila–but my quess is that it would be a source of FODMAPs.
Goose
Thanks. The agave would be high in fructose right? Also, one more question, would vanilla almond milk be high fodmap? Here are the ingredients
ALMONDMILK (FILTERED WATER, ALMONDS), CALCIUM CARBONATE, NATURAL VANILLA FLAVOR WITH OTHER NATURAL FLAVORS, SEA SALT, POTASSIUM CITRATE, CARRAGEENAN, SUNFLOWER LECITHIN, VITAMIN A PALMITATE, VITAMIN D2 AND D-ALPHA-TOCOPHEROL (NATURAL VITAMIN E)
….and one more question. Is coconut milk mainly used for cooking? Can someone have a glass of coconut milk without any negative health risks?
Thanks. I apologize if this has been answered before.
Jim
Hi Kate
Doc recently suggested FODMAPS diet due to a first recent bout with pain due to gas build-up. Have been eating a very small amount of Boar’s Honey Ham for breakfast with an egg on an English muffin for years at breakfast. I know honey is listed as a no, but do you think given the small amount I need to eliminate it at this time? No pain after breakfast but seem to have reaction after lunch and dinner. Was eating prunes daily and lots of pistachios so they are being discontued. Was hoping to keep the ham. Thanks, Jim
katescarlata
It’s hard to know exactly how much honey is in the ham. If you were my client–I might have you switch to a ham w/o honey –at least for a couple weeks–and then maybe try to add back the honey ham. Glad you pulled the prunes and pistachios out of your diet for now! They are very rich in FODMAPs!
Lisa
Hi Kate! I was just advised by my doctor to start a low FODMap diet and came across your website which seems very helpful so thank you. There are so many different lists out there (basically the same but a little different) my head is spinning! Anyway, my question is I see it says to limit celery to about 1 stalk. Celery and oranges have been the only thing I could really tolerate for the past 6+ weeks and I have definitely been eating more than 1 stalk at a sitting!! Do I really need to limit the intake of celery? I’m actually a little leery of eating anything else in public because everything has been giving me gas….the reason my doctor is suggesting this diet (along with Linzess). Thank you for your help! Lisa
patty
Hi Kate! Been on the low fodmap eating plan for just 1 week and noticing a very calm digestive tract. Today, however, I ate a nectarine – by mistake, I swear! I guess I was thinking orange/nectarine they’re all okay. But omg – within an hour or two, I’m wondering why I have gas? Haven’t had any all week. Then I went out shopping to try on winter jackets and vests and everything was fitting so tight. When I got home and looked in the mirror – went from 0 to 4 months pregnant within a few hours! Will this clear up quickly, or have I set myself back to square one? Thank you, Patty
katescarlata
Hi Patty, reactions to FODMAP sensitivities varies person to person–so I can’t tell you for sure how long it will take to calm your belly.I hope soon though!! Nectarines have both sorbitol and fructans–so you get a ‘double’ hit of FODMAPs. The combination of water being pulled in and fermentation of the FODMAPs by intestinal microbes creates gas–stretches the intestine. This gas and water can be trapped and cause visible distention–or the look of a pregnant belly. When this type of bloating is present in my patients, I do encourage they get screened for small intestinal bacterial overgrowth to be sure that is not part of their picture. This breath test for small intestinal bacterial overgrowth is called a lactulose breath test–some medical centers use a glucose breath test.
patty
Thank you Kate!
Anita Oleksy
I have been on FODMAP for about 6 mo. at the instruction of my GI Dr.
It has been helping.
I don’t *think* I am sensitive to almond milk – been using it for years, but now, I’m not sure. Cow’s milk tastes odd to me now, rice milk tastes nasty. What to do? I feel good – should I lose the almond milk and see if I feel *even better*? Maybe I’ve been blaming the wrong foods when I have *issues*?
Also, is a whole banana at a sitting too much?
Julie
Hi Kate!
I’m wondering if you can recommend an RD who knows all about FODMAPS in the NYC area?
many thanks! 🙂
katescarlata
Of course, Julie….I have some great colleagues I would recommend in NYC—Tamara Duke Freuman, Danielle Capalino, Tamar Samuels (at Top Balance Nutrition). Best to you!!
Kate
Sarah
Hi Kate!
Quick question for you. I’m really interested in starting a low FODMAP diet and I was just wondering if it would be okay to continue with dairy if I’m taking a Lactaid pill before having it? Also, do you have any thoughts on taking magnesium citrate supplements to help with IBS constipation issues? Thanks so much!
-sarah
katescarlata
Hi Sarah…I recommend avoiding lactose containing foods while embarking on the low FODMAP diet initially—most hard and aged cheeses are low enough in lactose to be included, lactose free milk –lactaid, Organic valley lactose free cow’s milk–would be okay too. And of course, Green Valley lactose free sour cream, cream cheese and yogurt works well for most patients. Once you have undergone the elimination phase–I might trial some lactase supplements with lactose rich foods. But, my preference for my clients–is to use them after the elimination phase.
sarah
thanks for the advice! that’s exactly what i figured would be best as well. what do you think about the magnesium citrate to help with IBS-C?
-Sarah
katescarlata
Oh yeah…sorry to miss the magnesium question. I am a FAN of magnesium….it works wonders for so many of my patients. Of course, discuss with your PCP before adding a magnesium supp to your plan. I love natural calm natural vitality–magnesium citrate–just add to warm water like a tea in the evening. I tend to start my clients slowly–1/2 dose for a couple days. Dosing is titrated to avoid diarrhea.
sarah
thanks! I’ll definitely discuss it with my GI doctor first. is there a certain time of day that’s best to take it for constipation relief?
-Sarah
Daniel
Hi Kate!!
I have a question regarding fruits: If I eat small amounts of the high-fodmap fruits such as half an apple or a slice of peach .. will it cause me the bad symptoms I always experience?? ..
How exactly does it work?? is it large amounts of fructose that make a fruit non-friendly with ibs sufferers like me? or is there a special component on these fruits that make them non-consumable?
Thanks!
katescarlata
Some fruit can contain multiple FODMAPs–apples have sorbitol and excess fructose. Depending on the type of peach–you might be consuming sorbitol or sorbitol plus fructans. When foods contain greater amounts of fructose compared to the glucose content in the fruit–the excess fructose can be poorly absorbed. And foods that contain multiple FODMAPs may contribute to greater symptoms as the malabsorbed FODMAPs effects in the intestine are cumulative. Tolerance to FODMAPs can be very variable–in those with IBS–so I would not say that a food is non-friendly to an IBS sufferer but rather a potential trigger food.
Holli
Someone recommnded to me a product called Intestinal Soothe and Build. The ingredients are: Slippery elm, marshmallow, plantain, chamomile, rose hips, and bugleweed. Do you have any knowledge of this product and its effectiveness for ibs, and are these ingredients fodmap friendly? Thank you!
Lisa
HELP! I thought I read on your website that corn syrup is ok but not HFCS. I just purchased your book entitled Low-Fodmap 28-Day Plan and on page 28 it lists corn syrup on the High Fodmap Food Additive List. Can you clarify this for me? It’s hard enough avoid HFCS but corn syrup too?! Thank you for your help. Lisa
katescarlata
Lisa, High fructose corn syrup is definitely not okay on the low FODMAP diet—regular corn syrup is a bit of a grey area—by definition–it should be okay–but testing it has been difficult. My current thought is to minimize it when possible–but I don’t remove it fully from my patient’s low FODMAP diet. My client’s eat foods that contain regular corn syrup without any issues. But it’s likely that corn syrup comes in many shapes and forms depending on how it’s manufactured. Bottom line: Eat more food created by Mother Nature and in the form she provides it to us–and you won’t need to worry so much about ‘corn syrup’. 😉
Khim
I am sure this has been asked before, but can you clarify where snow peas fall since they are listed in both the high and low (dose dependent) location on one of your handouts? Thank you! PS – your handouts are extremely helpful to my patients!!
Khim Schoenacker, RD, CSP, CD
Jackie
Hi Kate,
Is Ensure supplement drink fodmap friendly for someone with SIBO? The ingredients seem to be a bit unclear. Would you also remove all breads and grains or just try a regular fodmap diet first? thanks, Jackie
Jeani
I was wondering about Udi’s Gluten Free Florence Street Bakery “Farmhouse White Bread”?? Are there any ingredients that are not FODMAP friendly?
Thank you!!
katescarlata
Jeani,
I am not sure about the pea hull fiber. I would try it post the elimination phase to test your tolerance.
Rhiannon
There is very conflicting info out there about bananas. Some say unripe, some say ripe. Which version is low fodmap? Also, want to make sure plantains are low fodmap. I believe I suffer from SIBO, but also candida. Food reactions for me are instant. Instant gurling, instant bloat. I’ve struggled with trying to do it on my own for 2 years, since being diagnosed with UC. I’ve been paleo for 2 years, SCD for 1 year and now low fodmap(which i even react to some low fodmaps). I also struggle with exhaustion and ice cold feet! I do think it’s time for me to go see a natural doc. I just want to feel better.
katescarlata
Absolutely work with a health professional to help your sort out your food reactions and gut health issues! You may have another autoimmune condition playing a role in your symptoms. Has your thyroid function been checked? There is very conflicting data about bananas out the internet. I follow Monash University’s research–and neither ripe or unripe are a large source of FODMAPs. Ripening the banana breaks down the starch in it–which ups the glucose and fructose content—but even in ripe bananas the glucose/fructose ratio is suitable for the low FODMAP diet. Resistant starch can up the beneficial bacteria in the gut. But everyone’s tolerance to it is different based on the sensitivity in your gut, the gut microbes that reside in your intestine–and probably a number of other reasons yet to be elucidated in the research.
Denise
My dietitian told me that corn syrup solids were just a powdered form of HFCS, but that’s not what I’ve found when digging around on my own. I have been avoiding anything with corn syrup solids just in case but there are so many foods with it! Corn syrup is fine for low fodmap, but are corn syrup solids? I would love to be able to eat a hamburger bun at my favorite restaurant instead of bringing my own :/
katescarlata
Denise, per FDA–Corn syrup solids should be glucose based…not HFCS. I don’t encourage corn syrup or corn syrup solids in large amounts or in multiple foods per meal–but I do allow them in general.
Michelle
Hi Kate,
I am having trouble finding a low fodmap childrens multivitamin. (Hoping for one not full of sugar too of course). Do you know of any? Thanks for all you do!
Michelle
Michelle
Also, do you know of any fodmap knowledgeable dietitians/naturopaths/etc. In the CT (or second choice lower NY) area for a child? This is still new to our pediatrician.
Kris G
Great, informative website, Kate! At 51, I am new to this IBS world…I suspect it is hormone related. At any rate, I am wondering about the different FODMAP groups. I am just finishing the elimination part of the diet (been on it for 4 weeks now). As I begin the challenge phase, can you tell me which groups seems to be the most tolerable for people? (I know onions and garlic are one of the hardest.)
Kris G
Great website, Kate! Thank you! Quick question: Can you tell me which of the FODMAP groups seem to be most tolerable for people?
Sharon Williams
Hi Kate: 2 questions please:
1. Can you recommend a good RD in Calgary, Alberta, Canada?
2. I am so confused- my lactose free milk says it contains 8gm Sugar/cup and my Becel Margarine has no sugar listed -Yet your blog says that lactose free milk is ok and margarine is not! Can you please comment?
Taylor Hawkings
Hi Kate!! I’ve been on the low fodmap diet for about 2 weeks now and I’ve lost 10 pounds so far! I do have a question about puffed rice though. I have the Monash App and it lists puffed rice as having a moderate amount of oligos-fructans. What I don’t understand is why? We can eat rice but not a cereal where the only ingredient is whole grain brown rice. What’s up with that? As for multivitamins, you suggested the vitamin shoppe, but you only mentioned calcium citrate, magneseum, and vitamin d. Are we allowed to take multivitamins? I know the clinical consensus is that they don’t provide much in terms of minerals and vitamins, but still, I would like to know if there are ingredients or whatnot we should look out for when choosing a multivitamin. Do you have a preference? Thanks! I’m so glad I stumbled across your blog, you’re so helpful! 😀
katescarlata
Taylor…first of all I would try to slow down the weight loss to keep on the healthy track…2 pounds per week is a great goal. Foods can be altered in FODMAP content depending on the state they are in…it sometimes doesn’t see to add up…just as you noted that puffed rice does have fructans while regular rice is devoid of them! Grapes do not have fructans–but when you change them to raisins they do??! Ripeness can impact FODMAP content too. Food is complex. Yes, taking a multivitamin is okay. Just avoid those with added FODMAP ingredients–mannitol and sorbitol are often added. Basic maintenance by Metabolic maintenance is an option. I tend to recommend multis to be taken 3 times per week vs. everyday….with the focus of getting nutrients from food first.
Elizabeth
Hi Kate! I say hello from Germany, where the FODMAP-diet is just starting. Maybe I missed the information, but I would like to ask you about the Roiboos Tea. Would you consider it FODMAP-friendly? And is there more information about herbal teas available? I read that fennel tea is rich in FODMAP. Is there an explanation for that, as it is considered to be helpful with digestive problems. Thank you so much for an answer and greetings from Munich!
katescarlata
Hi Elizabeth,
Welcome all the way from Munich! A city I hope to visit in the very near future! I have not seen data on Roiboos tea. Fructans in the fennel tea can stimulate colonic movement via fermentation. Fructans are fermented into short chain fatty acids that can stimulate the colon to move. Unfortunately, fructans can also instigate IBS symptoms for those who are sensitive to them. It’s individual.
Monica
Hi there,
Wondering if you can recommend an RD in the Abbotsford, BC, Canada area who is knowledgeable with all of this. I have longstanding IBS and was diagnosed with SIBO last year, treated herbally which ended up being a gong show! My system is so messed up, I don’t know what to eat anymore! So I’ve been researching this on my own when I came across your site which looks helpful…. But I am so confused with all the info I am reading about AIP, GAPS, SCD and now FODMAPS – I need help in figuring out what to eat! I have bad GERD as well and have been on Nexium for almost a decade and want to get off! Thanks!
katescarlata
I am sorry, I don’t know of a dietitian in BC.
Rosalyn
I simply want to thank you for this blog! I appreciate all the valuable information so much! It has been extremely helpful.
katescarlata
Thanks Rosalyn!! 🙂 means a lot!
Rosalyn
Hi,
Could you please tell me if sauerkraut is tolerated on a low fodmap diet?
Thanks!
katescarlata
Rosalyn, tolerance to sauerkraut is variable from what I see w/ clients. But if made with common cabbage without added fodmap ingredients– I would consider giving it a try.
Laura
Hi Kate,
The dietician I see (Janelle S.- I believe you know one another) recently put me on low FODMAPs in an effort to ameliorate GI issues. Oftentimes due to oesophageal motility issues, I am required to supplement what I do not finish at meals/snacks. Unfortunately, as I imagine you’re aware, none of the common supplements are suitable for this diet. What would you recommend for supplementation?
Best,
Laura
katescarlata
Hi Laura, I am afraid I am not sure what supplements you are referring to–can you provide more details? Are you referring to ensure drinks etc.?
kate
I’ve been looking at a couple probiotics. One has a “proprietary polysaccharide complex” listed, and the other has chickpea extract listed. I’m guessing that the chickpea extract would be an issue, but would the polysaccharide complex be problematic?
kate
Hi – do you have any thoughts on these additives in the probiotics?
katescarlata
Kate can you expand on what you are referring to in probiotics?
kate
One has a “proprietary polysaccharide complex” listed as an ingredient. The other has chickpea extract listed. I’m guessing the chickpea extract could be problematic, but wasn’t sure about the polysaccharide complex.
Anna Soloff
Hi Kate,
I just stumbled across your blog. I have been quite ill with digestive issues mainly bloating, nausea, vomiting (all this as soon as I take a bite of food), fatigue…for the past 3 years. I have been tested and treated for many things, tried every diet imaginable without any relief. Do you know of someone in Illinois or even Indiana that you could recommend? Or any resources or disorders to consider?
Thank you!
katescarlata
Anna, have you been tested for delayed gastric emptying? With the nausea and bloating–this might be a good test. Also a gastric accommodation test might be another suggestion to run by your gastroenterologist. Perhaps, try Susan Allen via: http://www.parkridgemd.com
Anna Soloff
Hi Kate,
Thank you for the response. I’m 37 and have been sick since I was 33 and am quite frustrated as I’m sure you understand only too well. My gastric emptying was normal. In the past I was found to have and was treated for peptic ulcers, SIBO, pelvic floor dysfunction, IBS, candida, heavy metals, painful bladder syndrome, along with a few other things. Having a brain fog day. I will definitely look in to the gastric accommodation test! I am currently at Northwestern right now but will contact Susan Allen. Thank you so much again and please let me know if you have any other thoughts or suggestions 🙂
JEAN
Hello Kate,
I am trying the FODMAPS elimination diet for chemotherapy induced…..well, it acts like IBS, and I’m in the process of cleaning out the offending foods from my diet. I’ve been at this for four days now and I think I see some improvement in pain, at least.
This issue just raised its ugly head about a month ago, and advice from my oncologist for Beano and simethicone just isn’t making it.
I’m finding that in a lot of GF bread mixes that are almost FODMAP friendly, one of the ingredients is pea protein, a relatively new, I think, protein. Peas are restricted on some lists, although not on yours, do you think pea protein is a problem?
The other question I had involved tapioca flour, I remember tapioca as being relatively sweet, is it a problem in this instance?
Thank you for your time, I’ve read the whole comment string and it has helped a lot, not to mention your other literature.
I should say that I’m GF and mostly lactase free, I’ve done food elimination trials and I know what makes me sick……although I hadn’t ever thought of FODMAPS as a problem. I’ve managed my constipation all my life and it hasn’t impinged on my life very much. Not as some describe it.
Also, I’ve just started the B. infantis probiotic, which has decreased some of the pain I was experiencing, although I’m still blown up and looking four or five months pregnant.
Well, that’s enough for now, thank you again for your dedication to this problem.
Jean
katescarlata
Consider being checked for small intestinal bacterial overgrowth–which can contribute to that big bloated pregnant-like belly. I have not seen data on tapioca–but it is quite starchy so should be okay. Pea protein–hasn’t been tested. I find some products such as Go Macro bars with pea protein are tolerated by my low FODMAP following clients–but if you can find a bread without it—that would be best….to be sure.
kate
would a probiotic that lists a “proprietary polysaccharide complex” be problematic? Thanks for your time!
katescarlata
Polysaccharides are not FODMAPs–FODMAPs are short chain carbs and polysaccharides are long chain carbs.
alicia
Do you have any recommendations for a nutritionist well versed in FODMAPS in the Baltimore area?
Many thanks!
Rachel
Hi there, this is a very thorough and helpful blog! I was wondering if you know of any information which is UK based at all? Although all of the information is brilliant, some of the brands mentioned are not available over here. Also, are you allowed to eat lactose free chocolate at all? It is my only vice!!
Many thanks, Rachel.
katescarlata
Small amounts of chocolate are okay on the low FODMAP diet. 30 grams or about 5 squares per serve.
Nicole
Hi Kate,
I am looking for a FODMAP friendly multi-vitamin. I was looking at the ingredients for Vitafusion Women’s and it seems like it might be ok? I am not sure though…what are your thoughts?
Also, do you know of any good FODMAP experts in Chicago?
Thanks,Nicole
katescarlata
I do allow the Vitafusion’s Women vitamin. Seems to be well-tolerated. I don’t know of any FODMAP experts in Chicago–but I would imagine that U. Chicago Medical center has one–would start there.
Jonathan
Hi Kate, your blog has been so helpful for me and my girlfriend as we try to figure out stomach issues she has been having for the past year. She started the Fodmap diet a few weeks ago and it has been helping. We recently read somewhere that almond milk has not been tested for fodmaps and might not be friendly for the diet. This is what she usually drinks and so a few days ago she switched to lactaid milk. Once she started with the lactaid milk, she started getting very severe stomach pain. She stopped drinking it yesterday and the pain is gone now. Any idea as to why/how laictaid milk could cause that kind of reaction?
katescarlata
Could be the dairy is an issue for her. Some people can’t tolerate the protein in dairy. Can she tolerate cheese?
Jonathan
She doesn’t eat much cheese or other dairy really. She would have some in a salad or something once in a while but it doesn’t bother her much. The only other dairy she eats is ice cream (before this diet) and that would give her some discomfort but nothing like the lactose free milk did.
I am also wondering how do you introduce back in the Fructan and Polyol groups back in with so many overlapping foods?
Denise
Hi Kate,
I just found your blog and love it! …. I was recently diagnosed with IBS and have been following the FODMAP diet with some success. I do have a couple of questions though …. can you tell me if Almond Milk, Stevia and “Sachi Inchi Protein” (protein ingredient found in Raw Vegan Paleo Protein powder.
Many, thanks.
katescarlata
Denise, almond milk is likely high–but we should be getting some info on it soon–I know it was on the list of foods to be tested. Stevia is fine–but avoid stevia products with additives such as erythritol. And Sachi Inchi protein?? I have no clue –doubt it has been tested!!
Janys
On the FodMap diet can you have one half of a Granny Smith Apple a couple times a week……..having issues with not enough fiber. Thanks
katescarlata
on the elimination phase of the diet, Granny Smith apples would not be allowed. Work with your dietitian to address ways to boost low fodmap fiber!
Lane
I’ve been in the “elimination phase” for 11+ months. The two times I tried leaving the diet were so unpleasant I don’t want to try again. For that matter, I had a terrible three-week “relapse” even when I didn’t violate the elimination phase. Sigh. My “best” 10 weeks were when I stuck to the elimination phase and ALSO had no chocolate (will never have any again, and I was not eating any with milk in it).
My story sounds self-absorbed and boring!
I guess it’s forever, this diet….pretty limiting, and not healthful, but one does what one must. Quality of life rather than length! Still not symptom free, not a bit, but, nothing else has helped in all these years, soooo …onward! Keep plugging, all of you!
Samantha
Hi Kate,
I’m planning on trying the FODMAP diet and starting in a few days. I’ve been gluten free for a year and a half and that seemed to work miracles for the severe constipation I was having. Then I started experiences some symptoms again so I’ve decided to give this a whirl. I’ve done a good amount of research and met with a dietician. Can you tell me what kind of coffee creamers I can use? I usually use the different flavored coffee-mate creamers. I know they’re gluten free and dairy free. The one I have right now (coconut flavor) doesn’t have HFCS. If I can’t use those, is there something else you can recommend? Thanks so much!
katescarlata
I am not a big fan of coffee creamers in general—to much junk added to them! But maybe someone else might be able to weigh in!
Christy
Homemade coffee creamer might be helpful. There is a great recipe in Danielle Walker’s cookbook Against All Grain. You can personalize the flavoring with whatever works well for you.
Heather
I was just perusing this comment thread, hoping to find something helpful for coffee creamer. My FODMAP elimination diet came from Mayo Clinic and it says no milk (not even low fat varieties)… But yet you supposedly can have 2 Tbsp of Half and Half. That makes no sense to me. Not to mention, I drink a decent amount of coffee and 2 Tbsp just isn’t going to cut it! Haha
At any rate, I checked out the recipe by Danielle Walker, and sorry… but that’s just too much work. She had me until the “strain the boiled liquid through a cheese cloth” (and then it only lasts 7 days at a time). NOPE. Too much work for not enough product.
My solution: I just bought a container of the Silk brand almond milk coffee creamer (french vanilla flavor) at the store. I believe all the ingredients are okay in it (though please correct me if I’m wrong). No high fructose corn syrup or dairy at all. At least for the elimination diet I’m on, almond milk is limited to 8 oz per day. But even so, 8 oz equals 16 tablespoons. So even if you were to drink giant cups of coffee that require 4 Tbsp of creamer (*ahem*…haha… told you I LOVE my coffee!) – you would still be well within the limit drinking coffee throughout the day with this creamer.
I like my coffee creamy and sweet, so I used 2 Tbsp of the creamer for 8 oz of coffee, then added a 1/2 teaspoon of splenda as well. Not quiiiiite the same as normal creamer, but it’s darn close. I’ll take it! 🙂
katescarlata
What about this french vanilla almond milk creamer? http://sodeliciousdairyfree.com/products/almond-milk-creamers/creamer-french-vanilla
Brooke
Tums OK?
Ensure or Boost drinks OK? need something for weight gain
Thanks
katescarlata
Tums are made with calcium carbonate which can be constipating–so depends on the patient. Tums has numerous products so would have to comment specifically on individual products–the typical/orginal chalky formulation –should be okay in small amounts if constipation not major issue. I try to minimize use of products that reduce acid–if at all possible–as to not encourage bacteria to grow in the small bowel. Boost high protein is the best tolerated product in my practice…again–there are many products in the Ensure and Boost line–and I don’t allow all of them. And my preference is to always supplement first with whole foods vs. products. Products contain many untested additives/ingredients making their overall FODMAP content very variable and unknown.
Kathryne O'Hara
I am new to this diet, and it really seems to be helping. I have a question about “processed meats”. My brother-in-law makes his own bacon and sausage and is willing to change ingredients to be compatible with my diet…but I can’t seem to find anywhere that says what specific ingredients in processed meats are the culprits. I know onion and garlic, which are in the bologna, but not the sausage or bacon. But what else in there causes the problem?
katescarlata
Kathryne, the onion and garlic would be the mostly likely culprits in processed meats from FODMAP perspective.
Jenn
Hi, thank you so much for all this amazing information! Do you know if Yacon Syrup is high or low FODMAP? I use it daily and wonder if I need to eliminate. If so, what do you suggest as a sweetener for decaf coffee?
katescarlata
Hi Jenn, I am not a Yacon syrup expert–but what I have read, it contains FOS (a source of FODMAPs). Patients opt for pure maple syrup or just a small amount of sucrose or stevia as a sweetener for coffee.
Carol Belliveau
Kate,
You are a lifesaver…just started the diet…so appreciate the work you do and information you share.
Thanks,
Many Blessings
Carol
katescarlata
Thanks Carol. Glad you stopped by the blog and I truly appreciate you kind words!
is
Hello,
starting FODMAP diet for 5 weeks and wanted to know if anything in these 2 supplements is not allowed?
B12 – http://www.jarrow.com/product/58/Methyl_B-12
D3 – http://www.countrylifevitamins.com/store/vitamin-d3-2500-iu
Thanks,
katescarlata
Best to send me ingredients and I can give you some of my best educated guesses!
is
D3- medium chain triglycerides, gelatin, glycerin, purified water (capsule shell)
B12 – Xylitol, cellulose, stearic acid (vegetable source), natural lemon flavor, magnesium stearate (vegetable source), citric acid and silicon dioxide.
katescarlata
I would think the D3 would be okay. Glycerin may be an issue–but likely not in that amount. The B12 has xylitol–which I would suggest your avoid.
is
hi
what b12 chewable do you recommend that does not contain xylitol, most of them contain some sort of sugar?
thanks
katescarlata
Might try this liquid option—but discuss w/ your doctor as I it is not appropriate to make individual recommendations: http://www.thenatural.com/pure-encapsulations-b12-1-fl-oz-liquid.html?CAPCID=10856688414&CADEVICE=c&CA_6C15C=320012280000396829
Steven Hertz
Hi Kate,
Thanks for a terrific website.
I wish you can clarify oat bran cereal.
I see that it is treated differently than oat cereal; oat cereal has possibly 1/2 cup and oat bran cereal 2 tablespoons.
Is this accurate and why the difference.
I also noticed that there is a gluten free version of oat bran cereal, should that make a difference in the amount allowed.
I happen to like oat bran cereal and generally eat about half a cup and was wondering about your thoughts.
Steven
katescarlata
Hi Steven, Glad you stopped by my site. First, if you seem to tolerate the oat bran—then continue with it. Tolerance to FODMAPs is variable —-and listening to your body is key. If you are still symptomatic–then I might reduce the oat bran to 1/4 cups dry (same limit as the oats should be fine) per serving. In larger servings such as 5 tablespoons it is over the fructan/ GOS FODMAP cut-off. Not sure that Monash has tested gluten free oat bran vs. regular oat bran–so can’t comment if it would have less.
Farzana
Hi Kate, sorry if this has been asked already but I am trying to find a coffee substitute. I have just started in the FODMAP journey and I have SIBO. I used to start my day with a cup of bulletproof coffee but I found that it kept me but me buzzing all day (not in a good way). I swapped over to dandyblend but due to the chicory, which I understand is high FODMAP, I need to put that aside. I know people swap cocoa for coffee in these fatty drinks but it is not allowed on the SIBO protocol. Can you help? Any suggestions? TIA
Ashley
Hi Kate, I am so thankful for your website! I developed severe stomach issues as a response to a traumatic experience that happened to me last year. The FODMAP diet really seems to help ease the discomfort and your website has the best information! I made your Mesa Sunrise Cereal Bars with the mesa sunrise cereal, marshmallows, and peanut butter. I had a pretty bad reaction to these and I am thinking it may have been the marshmallows I used. Is there a brand you recommend? I used Kraft Jet Puffed (not made with HFCS but did have a “whipping aid”-not sure what that is). They were delicious so I would like to try and make them again! Thanks
katescarlata
Ashley–might have been too much sugar or too much fiber….sometimes other foods can be a trigger beyond the fodmap content. I typically use Whole food marshmallows. Not sure about Kraft. Also, if you find sugar is a trigger for you–you might consider talking to your doctor to see if small intestinal bacterial overgrowth might be part of your picture. Just an idea to discuss.
Ashley
Thanks so much Kate! I’m beyond blessed by your blog. Thanks for all the work you do.
Don Brown
Hello Kate,
I noticed Egg is an acceptable protein. Is it the whole Egg or just the white. Many
diets just specify the Egg white. What is your rational and how many a day can I eat.
Thanks for all your helpful information,
Don Brown
katescarlata
Eggs are not a source of FODMAPs. As for personal limits–it really is individualized per patient. In general, my clients enjoy 3-4 eggs per week.
Don Brown
Appreciate your response !
Justin F
Hi Kate,
I have been following a FODMAP free diet for 5 days and have noticed a huge difference to my gut health, but I am still confused with regards to nutrition for my endurance cycling. Historically, I ate, drank products loaded with fructose / glucose and maltodextrin. My favorite brand listed the following.
“It contains maltodextrin and fructose in a ratio of 2:1” From this I assume it means fructose is in greater ratio to glucose and therefore a poor choice if trying to follow FODMAP.
I have stumbled across another brand with ingredients that just read. Maltodextrin, Sucrose .. for the powder and Maltodextrin, sucrose, glucose syrup … for the energy gels.
Based on these ingredients would you say these too are off limits or a better option than my previous energy powder.
katescarlata
Not sure about maltodextrin–I do allow it–but I think it might be a wild card when it comes to FODMAP content. Perhaps you might find something that will work for you on my Pinterest: FODMAP runner board. The products have not been officially tested but might work: https://www.pinterest.com/katescarlta/fodmap-runner/
Justin F
Thanks Kate, I’ll take a look.
ron
Kate was wondering what is your belief or take on pea sprouts?
Jennifer
I stubbled across this on accident when looking up marshmallows as high in FODMAPS.
I’ve had IBS since I was 10… I’m now 25 and all the doctors do is say “it’s diet based” give me tablets for when i’m either unable to go or can’t stop going and just leave me to that… no dietician’s help… nothing!! I keep going back as I just can’t seem to understand the whole “diet” thing… like one day i’ll be fine the next I wont be.
I know gluten and dark greens is a huge trigger for me so I decided to go gluten free. A friend mentioned FODMAPS diet to me and so I decided I’d look it up and go alone with it. I know it’s probably the wrong thing to do BUT I have tried to get help for both weight and my IBS and the drs just result to pills (they did refer me to a dietician for my weight but once i joined WW I started losing again so I decided I didn’t need the appointment… maybe i shouldn’t gone just to see if she brought up an IBS diet… ah well)
I’m so thankful I found this page and I’ve now booked marked it to look at when ever I need help!! Finding it so useful!!!
Today is day 1 for me 😀 wish me luck!!!
katescarlata
Good luck Jennifer!!
Britney
Hi Kate,
The probiotics I just bought have gelatin in them. Are those okay to have? Having a hard time finding probiotics with low fodmap ingredients.
Thanks!
katescarlata
Gelatin should be okay, Britney!
Britney
Thank you!
Beth Ellen
Hi Kate,
First of all THANK YOU for your commendable work and desire to help others! I have a quick question… I saw in one article that green beans and fennel bulb were both sources of a number of FODMAPs (Muir et al doi: 10.1021/jf802700e J Agric Food Chem. 2009 ) but I don’t see a limit for them on your (awesome) low FODMAP grocery list https://blog.katescarlata.com/wp-content/uploads/2016/01/truefinal-groceryposter_jan2016.pdf. Is it possible new information has come out and they would be fine on a low FODMAP diet? Also I am having a hard time finding out if globe artichokes/artichoke hearts are OK on low FODMAPs. It seems the research was done on Jerusalem artichoke which I believe is quite different. ALSO would BEANO be useful for someone sensitive to FODMAPs in legumes/pulses, especially green peas? Thank you so much, Beth Ellen
katescarlata
Beth Ellen, I would suggest you purchase the Monash app to receive the latest info on how to apply the low FODMAP diet. The food lists have evolved and changed with research. Most produce has some degree of FODMAPs in them…the low FODMAP diet is NOT a FODMAP free diet–but rather a reduction of FODMAPs. I have not found beano to be particularly helpful in my clients—but you could give it a try.
MCD
Hi Kate, Love the blog!
My question: Can I take medication containing lactose despite being pretty sure I am lactose intolerant?
My specifics: I’m currently taking Linzess for IBS-C, but it has become less effective. A gastro doc recommended Resolor out of Canada, (http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/001012/WC500053998.pdf) and it does specifically say, “The tablets contain lactose. Patients with rare hereditary problems of galactose intolerance, the Lapp
lactase deficiency or glucose-galactose malabsorption should not take this medicinal product.”
I’m tempted to try it even though I have to pay out of pocket. However, when I have taken probiotics with lactose, my stomach has become upset.
I appreciate your insights!
katescarlata
I can’t provide individual advice in a blog setting, but the small amount of lactose in one pill should be okay for those w/ lactose intolerance. If you were taking multiple pills with lactose they could add up to be a problem. You could try a lactase enzyme supplement when you take the pill if you are concerned. It could be the probiotics you are reacting to rather than the lactose in the probiotic. That would be my initial thought. And have you been tested for methane gas in a small intestinal bacterial overgrowth test—I think this test would be a good idea in a person w/ worsening constipation.
jessie Jace
Are artichoke hearts ok?
katescarlata
Less than 1/4 cup is okay. But overall–on the higher side–w/ excess fructose.
Faz
Hi,
So glad I’ve found this blog.
I’m struggling! Just started an elimination diet 2 days ago- low fodmap, gluten free & dairy free.
I’m particularly stuck on how to ‘read’ food labels on various items to know which ingredients to avoid. For instance a gluten free bread I purchased contains: ‘Hydroxypropyl Methyl Cellulose’ ingredient names like this always confuse me & put me off.
Lacto free cheddar vs standard cheddar cheese? Is there a point in purchasing the former given the little lactose in the latter?
Is coconut flour high or low fodmap? I see it being used in baking recipes alot.
I feel VERY limited as have been brought up eating garlic & onions, almost all our dishes contain these & I’m now having to avoid them! 🙁
I’d appreciate your advice. Thank you for your time.
Many thanks 🙂
katescarlata
Try to minimize products and eat whole foods for starters. The list of ingredients can be daunting. Cellulose is not a FODMAP—but methylcellulose in animal studies shows it can increase bacterial overgrowth and inflammation. Most cheese that is firm is low FODMAP–the lactose in cheese is in the wet part of the milk–so ricotta and cottage cheese would be higher FODMAP. Try using some garlic infused oils in your favorite recipes–these are low FODMAP and flavorful. My fav is Boyajian garlic oil.
Caroline
Hi Kate, I am noticing confliction between some of the Fodmap food items you deem acceptable compared to that of other sources that have provided references. Can you confirm the following foods are acceptable with your explanation / source?
Potatoes, table sugar and beer, to name a few. I have not scrutinized the entire list, but I am feeling a little skeptical about the entire list at this point. Normally I do not bother commenting, but it is differences like these that make people confused. By no means am I stating you are not incorrect, would simply like justification why your information is different. Thanks so much!
Caroline
Sorry, what I meant to say above is: by no means am I stating you are incorrect as opposed to not incorrect.
katescarlata
I understand your frustration, Caroline. I follow the pioneers of the low FODMAP diet at Monash University for my data. A good resource for you would be the Monash University low FODMAP diet app. Table sugar, white potatoes and beer are low FODMAP per Monash research. Not sure what others are posting on their blogs. I don’t always provide resources on my blog—truthfully, as the blog is something I do in the very very few minutes of free time I muster up each week. It is truly a labor of love but one I felt people with IBS needed to help provide sound nutrition for the low FODMAP diet. Try to find a dietitian to guide you. And remember most people simply need a reduction of FODMAPs rather than a super strict diet. Additionally, beer may be low FODMAP but alcohol is a gut irritant–and too much alcohol can pull water into the gut. So…there is more to gut health and symptom management than the low FODMAP diet. The other issue with the low FODMAP diet is that is it relatively new–and evolving. The food lists get up dated regularly.
Karole
I was given the FODMAPS diet sheet to try. Then I was tested positive for SIBO but was given no direction. So tried to stick to FODMAPS. Finally saw dietitian (no FOADMAP/SIBO specialist in my area) gave me FODMAPS/SCD sheet to follow. So lost. Been trying for weeks to get on a nutritional trail to feel better. Have other health issues (COPD) so really need good nutrition. Any suggestions. Also need to take complete B, D3, magnesium and get potassium rich foods due to fluid pills.
katescarlata
I don’t typically instruct patients with SIBO to do the combo SCD and low FODMAP diet—it is too restrictive–especially for someone that needs the extra calories and well balanced nutrition. Unfortunately, it is impossible to truly weigh in on your case in a blog setting!
For my SIBO patients, I typically start with a low FODMAP diet w/ adequate spacing between meals–3 hours ideally to allow the migrating motor complex in the small bowel to initiate a cleansing wave, which it will do when you haven’t eaten in a while. There are many potassium rich foods allowed on the low FODMAP diet–bananas, potatoes, tomatoes for starters. Magnesium rich foods include hulled pumpkin seeds (pepitas), quinoa, peanut butter. D3 is typically taken via supplement–as there are few food sources. Are you being treated for SIBO w/ an antibiotic? Some patients do seem to need some additional diet modifications w/ the SIBO–but it truly varies person to person. But, adequate nutrition is essential for your overall health –so be careful not to be too restrictive!
Judy Dent
which is best for SIBO sufferers…real cream in their coffee or non dairy creamer? I just can’t give up my morning coffee with cream!
katescarlata
Great question, Judy and I can’t answer it with authority as their isn’t much study around diet and SIBO, unfortunately. I might opt for using light canned coconut milk perhaps. Or small amounts of real cream. The non dairy creamer products often have so many additives.
Gail Schneider
Puzzled about something – I downloaded the Monash Fodmap App and it says Eddamame (cooked from frozen) is ok at a one cup serving. I wouldn’t eat that many but I thought from one of your comments here that soybeans were high fodmap.
katescarlata
Hi Gail, I had the same question, when I saw the update. Edamame –immature soybeans– appear to have less FODMAPs than mature soybeans, so a few pods of edamame–up to 1 cup in the pod, is low FODMAP. Soybean in general is one of those very confusing foods in the world of FODMAPs as depending on the processing –FODMAP content varies. For instance, firm tofu–is low FODMAP while silken tofu is high. Soy sauce is low FODMAP. Soy flour contains FODMAPs. Soymilk made with soy protein alone is low FODMAP–while soymilk made with the whole soybean is high FODMAP.
jmke
Re the FODMAP status of cassava –
Monash University tested fresh cassava in March 2016 and found it, in “typical serving sizes”, to be High FODMAP (https://fodmapmonash.blogspot.com/2016/03/research-update-fermentable.html).
As far as I can see their flour lists don’t comment on cassava flour but it might be something to be cautious about.
Barbs
Hi, thank you for this fantastic resource, it is truly appreciated. Can you please tell me if aloe vera juice is ok to drink? Thanks 🙂
katescarlata
I have not seen data on aloe juice–but many patients with constipation do try it –doesn’t seem to aggravate symptoms. When products are not tested for FODMAP content–its’ best to trial them in small amounts w/ guidance from your dietitian.
Bonnie
Hi Kate.
I have read with interest this entire blog post including all the comments. I have been on the low Fodmap for a few months but I have never done the re-introduction phase. I am gluten intolerant (2.5 years) yeast intolerant and even though I am on the low Fodmap I still have issues with bloating and gas most days. I have been to see someone who suggested I go off 7 things for 3 weeks and then re introduce them one at a time over 3 days: 1)gluten (already off) 2)sugar (already off all sugar-including all sweetners, except erythritol which doesn’t seem to affect me at all) 3) Corn 4) peanuts 5) soy 6) dairy 7) eggs. I am on day 4 of this elimination diet. Day one and two I had headaches and mucus in my throat which is gone day 3 and 4. In fact I have a lot more energy than I have had for a long time . My bloating has been much less although not completely gone yet although this could be to maybe it still being in my system? However today was different. I ate the same food I have been eating all 4 days except for tonight I had grilled white fish with no spices at all and hot potato chips. Within an hour I was hugely bloated and had gas. However both fish and white potatoes are listed as low Fodmap. Do you have any ideas on this? Also I don’t understand why some food that are listed in the same family group like for example cruciferous vegatables -broccoli and cabbage is listed as green on the Monash app but cauliflower is listed as red but all belong to the same family. All have an enzyme in them that produce gas when in the colon. I cannot eat any of these from that family group, including brussle sprouts and turnips(which is also listed green). Why would some be okay and others not? Or is it just dependable on the person and their specific gut reaction?
I appreciate any suggestions you may have regarding these two things.
katescarlata
I would recommend you work with a dietitian knowledgeable in digestive health to guide you. Sometimes–you may experience bloating due to reasons outside of what you are eating—constipation, for instance is a risk factor for bloating. Fish could cause symptoms in some people due to histamine content.
Tori
I have recently started Shakeology and I drink the Vegan Chocolate Shake. I have been trying to research and find out if it is FODMAP approved. What do you think, and thanks for your help.
katescarlata
Tori,
Send me the list of ingredients and I can provide an educated guess. Unless a product is analyzed I can tell you for sure–but the ingredients can be a good general guide. ~Kate
Dyan Brinkman
Wondering if you were able to look into Shakeology being FODMAP approved yet? And if so what your findings were. I have been drinking it on and off and noticed that when I drink it I have some pretty significant gut issues… Would love to hear what you found out.
katescarlata
I haven’t looked into these shakes—but it sounds like your body is letting you know they don’t work for you.
vincenzo
hy kate, What about roaste chicoree coffee? is it low or high in FODMAP?
thank you
vincenzo
katescarlata
Sorry for the delay–not sure that I have seen info on chicory based coffee.
Amy
kate- any thoughts on marshmallow root taken as tea?
Thank you!
Amy
katescarlata
No idea, Amy. Doubt it has been tested.
amy
So far so good! It has actually been super helpful, and I’ve read that it repairs mucilage in the gut. Maybe check it out!
Thanks Kate!
Amy
Hi Kate, I am hoping you might have experience with this. I’ve had worsening ‘IBS’ for years (with diarrhea). In the last two years it has been associated with weakness, feeling faint and occasionally fainting or collapsing, flu-like symptoms, severe brain fog, depression and generally feeling very unwell. I started fodmap free diet 6 months ago and it helped – I went from 15 immodium tablets a day to 2. But I was still having to go to bed after a bowel movement because I feel so terrible. Now I’ve been diagnosed with SIBO. I have no vitamin deficiencies (all my blood serum results are normal-high) and yet I haven’t seen anywhere that SIBO causes people to become so ill that they become really ill and unable to work (like me). I am not dehydrated either. In your opinion/experience can SIBO make someone REALLY ill or is it just gastrointestinal symptoms ( right now I would do ANYTHING to go back to the days when the only thing wrong was my stomach 🙁 I am taking Rifaximin with guar gum right now and feeling worse but maybe because it’s working? Will be starting low dose naltrexone as a prokinetic afterwards for 6 months plus strict fodmap diet.
katescarlata
I might talk to your doctor about the possibility of mast cell activation syndrome. ARe you working with a progressive GI doctor?
ELIZABETH MARTINEZ
Hey, do you know if the nature made brand of vitamin C is considered low fodmap? If not, what multi vitamins…especially vitamin c. Can I get that are fodmap friendly?
katescarlata
Most of the Nature Made vitamins are good that I have checked. It would be best if you provided the ingredient list so I can weigh in.
Kate
Hi Kate,
I was told by my dietician that the rice milk (Rice Dream original, organic) I have been drinking is high FODMAP. But she also told me serving sizes (like 1/8th an avocado or 1/2 cup of oatmeal) is per day and not per meal/spaced with 3-4 hours in between as I had understood. Which is true? She also told me to cut out all dairy as I’ve been on the elimination phase for 6 weeks with no difference. Do you recommend non dairy milks (with brands) apart from almond (as I don’t like), or anything with pea protein or soy (I’m allergic). Thank you!
katescarlata
Hi Kate, The Rice dream organic original milk looks low FODMAP per ingredients. The serving size ‘cut offs’ of food is per meal –not per day. If you didn’t notice improvement on a low FODMAP diet–and you are sure you followed it correctly–for 6 weeks–I would think the next step would be to STOP the diet. If going dairy free didn’t offer benefit–again, I would not continue…BUT, sounds like you might need a more informed dietitian –or consider other treatment considerations–of course, I don’t know your full story–so discuss further with your GI doctor.
Shannon
My daughter was just put on a low fodmap diet due to SIBO. We have a road trip coming up. Any suggestions for how to eat at restaurants or fast food?