Well, Happy Monday! Despite the snow last week, I think Spring is really trying to arrive here in New England.
I thought I would kick off this work week with a deep dive into the topic of diarrhea. Sound good? 🙂
If you know me, you know I don’t mind talking about poop. There are many people that don’t feel the same way –ha! …and that’s totally okay. 😉 Some folks have suffered so long with diarrhea–that they simply expect to experience it every day. My response to this…”it’s not okay to not feel okay.” And experiencing diarrhea every day may simply mean your doctor has more exploring to do.
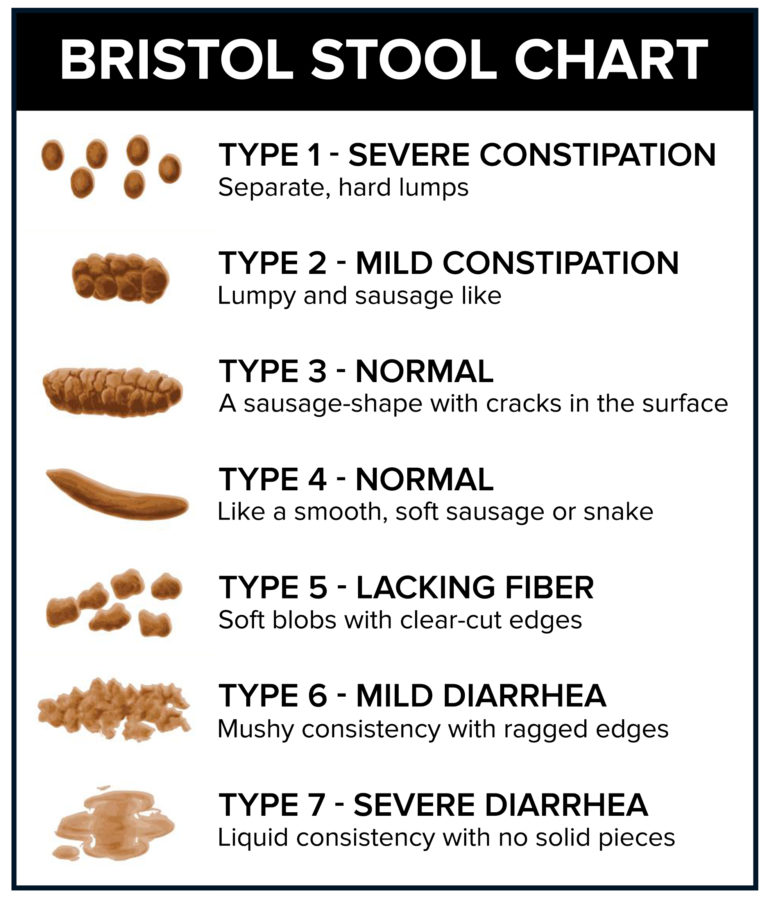
Chronic diarrhea (without co-occuring abdominal pain) occurs in about 4-5% of people living in Western countries (1) and is defined as a persistent alteration of stool consistency with loose stools (consistency between types 5 and 7 on the Bristol stool chart) and increased stool frequency of greater than four weeks’ duration. (2)
Where does your poop look like these days? Ideally, a stool in category 4 is a good goal for most people.
Alarm signs associated with diarrhea include: blood in the stool, black stools, severe pain, fever and/or unintentional weight loss. These signs or symptoms should be addressed immediately with your physician.
Diarrhea may present without these alarm signs but still occur on a daily or near daily basis. Always communicate your ongoing symptoms to your doctor. He or she will then investigate your chronic diarrhea based on a clinical differential diagnosis. More common or more serious conditions are generally ruled out first such as: celiac disease, hyper-or hypo-thyroidism, inflammatory bowel disease, irritable bowel syndrome and colorectal cancer.
Some initial screening blood tests may include: an anemia panel, thyroid function tests, c-reactive protein (to assess for inflammation), celiac serology tests (you must be consuming gluten for celiac screening tests to be accurate). Stool tests such as parasites tests (particularly if you drink well water in a rural area or have traveled overseas in higher risk areas), C. difficile (particularly in someone that has recently taken antibiotics), as well, stool calprotectin or lactoferrin, may be done to screen for inflammation in the digestive tract. Note: chronic diarrhea may occur in up to 10% of patients after their gallbladder is removed (cholecystectomy). (3)
Colonoscopy with biopsies of right and left colon can help exclude microscopic colitis, an inflammatory condition of the colon that requires biopsies to be identified. (3)
When fat malabsorption is suspected (which is often accompanied by odorous, pale colored stools or obvious fat in the stool), a fecal elastase test may be ordered to assess for pancreatic exocrine insufficiency. Small intestinal bacterial overgrowth (SIBO) can contribute to fat malabsorption as well. In SIBO, fat malabsorption may result as microbes present in the small bowel can impact negatively bile acid metabolism. Bile plays a key role in fat digestion. SIBO is generally assessed via a lactulose or glucose breath test. Some physicians opt to empirically treat for SIBO (with specific antibiotics) vs. doing a breath test as breath tests for bacterial overgrowth are not particularly accurate.
Other common conditions associated with diarrhea, include irritable bowel syndrome (IBS) with diarrhea predominance, lactose intolerance, bile acid diarrhea (read more on bile acid diarrhea here) and for those who have experienced abdominal or pelvic area radiation treatments, post radiation diarrhea. (3)
Can diet, supplements or medications impact the onset of diarrhea? Yes.
Overconsumption of alcohol can have toxic effects to the lining of the gut, increased risk of small intestinal bacterial overgrowth, can lead to pancreatic insufficiency, as well as prompt rapid intestinal transit. Too much caffeine can increase intestinal motility and too many FODMAP carbohydrates–such as lactose, excess fructose and sugar alcohols may increase diarrhea risk as well. Acquired or congenital sucrase isomaltase deficiency (CSID) may result in diarrhea with the consumption of foods and beverages rich in sucrose such as pastries, cookies, soft drinks, apples, oranges, pineapple, to name a few. Consider this diagnosis if consumption of sugar-y desserts or beverages prompt diarrhea regularly and/or traditional treatments for IBS such as low FODMAP diet do not work. In CSID or acquired sucrase isomaltase deficiency there is a decline in the digestive enzymes complex that helps digest sucrose and some starches. This may be due to inflammation in the gut or genetics. (4) Some dietary supplements such as those with high doses of magnesium, some medications such as anti-hypertensive medications and some diabetes medications may play a role in the onset of diarrhea as well. (3) Review your medications and diarrhea risk with your pharmacist, doctor or dietitian.
Experiencing diarrhea occasionally is normal. GI symptoms are common in humans. But, experiencing diarrhea on a consistent basis should absolutely be included in the dialogue you have with your doctor. Advocate for yourself so that you can feel your very best!
- Talley NJ et al. Onset and disappearance of gastrointestinal symptoms and functional gut disorders. Am J Epidemiol 1992;136:165-77.
- https://www.uptodate.com/contents/approach-to-the-adult-with-chronic-diarrhea-in-resource-rich-settings/print?topicRef=2000&source=see_link accessed April 14, 2021.
- Arasaradnam RP et al. Guidelines for the investigation of chronic diarrhea in adults: British Society of Gastroenterology, 3rd Ed. Gut 2018;67:1380-1399.
- https://www.gihealthfoundation.org/CME_offerings/eSupplements/CSID_Mono_Oct2020/CSID_Mono_Oct2020.pdf accessed April 19, 2021.

Lauren Bass
Can you recommend a gastroenterologist in the area who understands IBS? I live in Ashland, Massachusetts.
Thanks
katescarlata
Sonal Ullman at BIDMC-Needham, Alison Goldin at BWH-south shore, Brett Hassan at Milford Gastro Associates are a few.