Hi Friends,
First and foremost, I want to be clear about the image in this post, I am not the author.
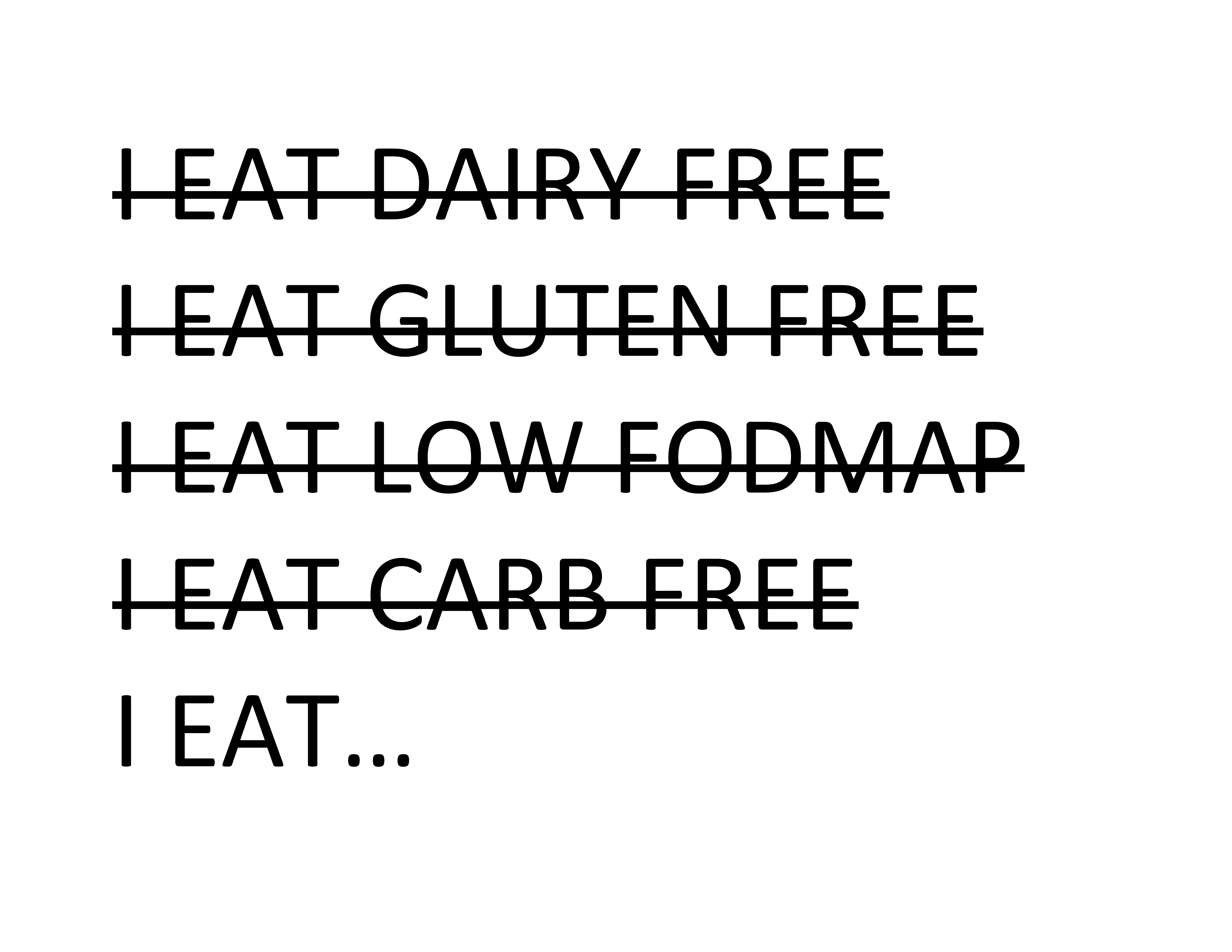
I put this image together after seeing a t-shirt with a similar saying, as well as many social media posts with similar messages.
I recently posted this picture on my Twitter feed to hopefully inspire some thoughtful discussion about how words matter. What we say can have very different meanings to different people.
I decided to engage in this same topic here on the blog.
How does this feature image make you feel? What does it make you think?
I welcome your responses in the comment section.
Some responses I received via Twitter about how this image made people feel included:
- Judged.
- Feelings of shame.
- People can be cruel about your food choices.
- My diet is both restrictive and freeing at the same time. But the judgement from others is more frustrating than the actual diet itself.
- People tend to make the assumption that I’m picky or fussy, or a health nut, but actually I LOVE food…
- I think this makes a lot of sense, if you are making the assumption that the person who wrote it was cutting out things based a trend…
Here are a few of my thoughts when I read this picture…
While I welcome messages that remind us NOT to restrict our diet unnecessarily–I think the delivery of such messages via this picture is coming from a very limited, privileged and biased place.
Let’s imagine you could not eat gluten due to celiac disease or otherwise and dairy foods contributed to intractable constipation. Now look at this list. I hope you might feel a bit more compassionate and understanding of this person’s diet choices.
I do welcome the notion that we don’t get hung up with food trends and pseudoscience –or overly restrict our diet due to recommendations that are not science-based. I personally embrace the fact that what we choose to eat is our individual right.
For me, I believe food offers more than a pile of nutrients. My goal of eating always includes the enjoyment of the flavor. I love to eat nourishing foods and foods that innately make me feel well. I am a fan of “pretty” foods too…a smoothie bowl carefully layered with fruit, seeds and nuts or a decorated chai latte–the aesthetic of the presentation makes my meals even more fun for me. I might add, I enjoy a sweet treat almost every day–which makes me really happy. 🙂 Raw onions, well, they fail me every time. And, I kindly ask that you don’t judge me for avoiding them.
There are many factors that inform what we eat. Our finances are certainly one of them. The degree of pain we may experience from eating is another. Religion and sustainability for our planet, are other factors.
Because food is something we have control over, I do feel many–and certainly not all— people with chronic GI disorders (from my clinical experience) have the tendency to be hyper vigilant about their diet. And I also find in clinical practice that this strict level of self-induced restriction is often unnecessary. Diet, of course, is just one modifiable factor to manage GI symptoms. Over restriction and hyper vigilance with the diet can add significant stress and a sense of deprivation. One can not undermine the impact of a strict diet on lifestyle, overall nutrition, the gut microbiome, and even GI motility. We also know that the gut microbiome can change with stress and under-nutrition. It’s a bit of a balancing act.
Today’s food culture is a bit crazy too. Food choice has become a moral issue. The villainization of food is not new. Gluten, for instance has been villainized in the media, and gluten-free foods has significantly increased over the last 30 years. Despite little science to support going gluten free for the vast majority of people in the US, “More than $15.5 billion were spent on retail sales of gluten-free foods in 2016, which is more than double the amount spent in 2011!” Reference: Statista. Gluten-free and free-from food retail sales in the United States from 2006 to 2020 (in billion U.S. dollars) [Accessed January 17, 2018]. https://www.statista.com/statistics/261099/us-gluten-free-and-free-from-retail-sales/ Published June 2013.
But how do we learn to eat intuitively in a world that is constantly bombarding us with food-fear based messaging?
I believe food intolerance occurs in many with IBS–and that diet modifications in many can offer relief. I do not believe that diet is a one-size-fits for all with IBS.
And here are some other thoughts to ponder:
Eating disorders impact ~2% of the US population. (Prevalence of anorexia nervosa in the US occurs in (0.8 %), bulimia nervous (0.3%), and binge eating disorder (0.85 %). Ref: Udo, T, Grillo G Biological Psychiatry 2018: 84(5):345-354.)
Of those with an eating disorder, about 90% will experience digestive distress and meet diagnostic criteria for a functional gut disorder. Read more here.
IBS occurs in about 15-20% of people in the US. Not everyone with IBS has an eating disorder. To learn a bit more about the prevalence of eating disorders in IBS, a recent survey study presented at Digestive Disease Week took a closer look at the relationship. The survey was completed by 91 adults with functional gut disorders (74% women). Eating behaviors were measured by the Eating Disorder Examination Questionnaire (EDE-Q) and the modified ARFID Canadian Pediatric Surveillance Program Questionnaire (CPSP).
Quoted in this recap of the study found here, “Overall findings: 22% of those surveyed has a low score on the Eating Disorder Examination Questionnaire signaling a likelihood of having a classic eating disorder, Dr. Zia, the author of the study. ‘This is not just restricting foods because of a fear of symptoms; this means having body dysmorphia.’ Roughly one-third (35%) met the criteria for Avoidant Restrictive Food Intake Disorder (ARFID)”
What is ARFID?
According to the www.nationaleatingdisorder.org, “Avoidant Restrictive Food Intake Disorder (ARFID) is a new diagnosis in the DSM-5, and was previously referred to as “Selective Eating Disorder.” ARFID is similar to anorexia in that both disorders involve limitations in the amount and/or types of food consumed, but unlike anorexia, ARFID does not involve any distress about body shape or size, or fears of fatness.” Additionally, AFDID criteria includes:
- An eating or feeding disturbance (e.g., apparent lack of interest in eating or food; avoidance based on the sensory characteristics of food; concern about aversive consequences of eating) as manifested by persistent failure to meet appropriate nutritional and/or energy needs associated with one (or more) of the following:
- Significant weight loss (or failure to achieve expected weight gain or faltering growth in children).
- Significant nutritional deficiency.
- Dependence on enteral feeding or oral nutritional supplements.
- Marked interference with psychosocial functioning.
- The disturbance is not better explained by lack of available food or by an associated culturally sanctioned practice.
- The eating disturbance does not occur exclusively during the course of anorexia nervosa or bulimia nervosa, and there is no evidence of a disturbance in the way in which one’s body weight or shape is experienced.
- The eating disturbance is not attributable to a concurrent medical condition or not better explained by another mental disorder. When the eating disturbance occurs in the context of another condition or disorder, the severity of the eating disturbance exceeds that routinely associated with the condition or disorder and warrants additional clinical attention.
If you read about ARFID, as outlined above, and the diagnostic criteria resonates with your eating experience, a referral to a GI dietitian and GI psychologist may be the best next steps.
Again, for a brief review of the study and finding, click here. Also be sure to read the interpretation of the study by Olafur Palsson as his points out some very valid and important points about this study.
One key point in this article noted by Dr. Palsson is: “The high prevalence of eating-associated problems in FGID patients that is reflected by the findings of this study underscores the need for people with such problems to receive a referral to a dietitian. Dietitians with GI expertise can likely help these patients identify specific trigger foods and guide them in altering their eating patterns in ways that can minimize eating-associated GI symptoms and help them maintain adequate nutritional intake.”
Here’s my bottomline:
Shaming is wrong: Whether that be “fat or skinny” shaming, general food or food intolerance shaming or whatever. Choose your words carefully. You have no idea what a person is going through. And if you are a victim of ‘food shaming’, it’s okay to speak up for yourself.
Food is not a moral issue: food is not right or wrong, unhealthy or healthy, good or bad. It’s food. Please just leave it there. Eating a brownie does not make you a bad person. I also dislike the word ‘cheat’ related to food.
Online resources geared toward individuals with IBS and SIBO are full of pseudoscience. People with chronic symptoms can be vulnerable to non-science based messaging–because they do not feel well. Just be careful who you trust. Work with a GI dietitian, if possible.
Do not over-restrict your diet unnecessarily! Try not to hold a grip on strict diet rules that do not serve you or are unrealistic. Try your best to eat a balanced diet that brings you joy as well as nourishment. Wellness includes the well-being of the body AND the mind. If eating a cupcake brings you happiness–than that too–offers some health benefits, in my opinion. Can you loosen up your diet restrictions and still feel well? Are your diet modification allowing you to have a more fulfilling life or are they limiting your life even more?
Please don’t make assumptions about people’s diet choices. You have NO idea why someone may or may not be eliminating some foods. Mind your own plate. This is an important message for health care practitioners, friends, partners, etc. We all have our own bias. Just be sure your bias doesn’t come off as privileged, slanted, or entrenched in a believe system that may work for you…but is disrespectful to someone else. If you are a healthcare provider, of course, it’s okay to ask about food choices in a non-judgmental way to ultimately help understand the rationale for a limited diet, and then when possible, help gently guide your patients to a more varied diet.

Holly
I thought that it was saying that we all eat, each to their own requirements and taste – no judgement needed. Crazy that our food traditions, preferences or necessities are often negatively labeled.
Looking at a list of hundreds of ethnic slurs on wikipedia (https://en.wikipedia.org/wiki/List_of_ethnic_slurs) it seems people have a nasty tendency to deride and judge “others” often using labels for food preferences or customs. For example, what comes to mind when you think of “hillbillies” and stereotypical foods associated with them? Reading a book from the PBS Great Reads list (Bless Me, Ultima) in which the young main character was teased for eating seasoned filling and tortillas while others ate sandwiches.
Thanks for this, Kate. It reminds us that many labels and judgements are untrue and unhealthy, sometimes including the ones we give ourselves.
Camille Sackett-Wescott
To me it means to focus on what I CAN eat versus what I can’t. I catch myself saying, “I can’t eat that.” Really, I could eat it. I’m choosing to keep my stomach comfortable rather than eat that particular food. So I’m trying to say something like, “I’m better off if I don’t eat that.” It changes the way I feel about the diet, too. I’m focusing more on taking car of myself instead of feeling sorry for myself for what I can’t eat.
katescarlata
Great attitude and perspective. Thanks for sharing, Camille!
Esther
Kate ..
This is a really great post ..! !
I often struggled and stressed when dining out ..
I had many food intolerances and most often felt embarrassed when using the words plain .. no sauce .. no dairy .. olive oil is fine etc .. This was true no matter if it was an upscale restaurant or not .. Often the chef or the waitress would come back and question me in front of everyone … Ugh ! I didn’t like drawing attention to myself while others listened probably wondering why I had so many restrictions or making their own assumptions .. If only the chef or waitstaff could hear me and simply bring me grilled or broiled .. baked or roasted potato and a vegetable if they had a low fodmap choice without asking me so many questions in front of everyone .. I often tried calling ahead and sometimes that would work but more often than not it didn’t ..
Overall I felt embarrassed and uncomfortable .. I would often say I have a sensitive digestive system not wanting to discuss IBS and SIBO over dinner and hopefully the conversation would move on to another subject ..
Sadly .. Judged .. feelings of shame .. stressed and more all applied !
Update ..
My diet has improved over the last couple of years or so … I no longer have as many food sensitivities/restrictions these days but still can’t tolerate milk/most dairy products .. It’s less of an issue for me but it’s still stressful and uncomfortable for me.
Thank you Kate for putting a spotlight on this subject ! !
katescarlata
Thanks for you comment, Esther! I appreciate you chiming in and sharing your experience–that many others have experienced too!
Sherry
… I eat ALOT…. and the food I eat now on the Low Fodmap diet is wonderful compared to what used to eat. I have learned how to modify most recipes to make them low fodmap and enjoy a wide range of foods.
Michelle
I’m wondering if you could speak about the AIP eating regimen and how that fits into the FODMAP way of life. I’ve been following FODMAP eating for a couple of years but recently had a big inflammatory flare up that now has me incorporating AIP too. I will see a nutritionist to help me navigate both but wondering who else lives with this and your opinion/experience with AIP.
katescarlata
I’m not sure the AIP is science-based.
Amy
Can I get “Mind Your Own Plate” printed on a t-shirt?! 🙂 LOVE that!!
I was recently caught off guard when I experienced some very judgmental comments about my own “picky” personal food choices and, more generally, about “those kind of people who eat fad diets like gluten-free.” Ugh. The person went on to say that the “supposed need” to eat gluten-free is “new” and that there was no such thing when they were young, that “kids ate peanut butter on bread every day and nobody died.” 🙁 Wow. What do you say to that? I tried to provide a bit of education, but soon gave up and walked away.
For me, the low FODMAP diet has saved me from so much pain and misery. As mentioned above, it allows me to focus on what I CAN eat! I still struggle occasionally with tummy troubles, but at least now I can generally trace the problem back to something I ate at a restaurant with questionable ingredients – and more importantly, I know what I need to do to get my tummy back on track. Before finding the low FODMAP diet, I was quickly reaching a point where I was afraid to eat anything because it seemed like EVERYTHING caused me pain and problems. 🙁 Many think that starting the elimination phase is daunting and overly limiting, but to me it was such a relief!!! I finally knew there were foods I could eat and had some guidelines that helped me get back to some sort of normal. I am so thankful to Kate Scarlata and this website/blog. The recipes and informative posts on here and in Kate’s book have really helped me on my FODMAP journey!! Thanks, Kate!
katescarlata
Maybe we need to make up some t-shirts! I am SOOOO…. glad you feel better. It’s sad that many people are uninformed about food intolerance OR are only able to see things through their biased and privileged lens. It must be nice to eat anything you want without consequence.
AnnMarie Anderson
Any ideas for speaking up for myself? I usually say “I love ______, but it doesn’t love me!” Sometimes I get a bit “riled up” when people make snarky comments…..
katescarlata
I love that response–and I would leave it there. You could also say, “how lucky for you that you can live well without food intolerance. It’s difficult at times when eating some foods leaves me in significant pain.” Just do your best to ignore the attempts of shaming or discounting your food intolerance.
Anita Oleksy
Some foods make me *hurt*, that’s all. If a food doesn’t cause a problem for another person, they have a hard time understanding that it might cause a problem for someone else. It took me a while to get my husband trained! Now he understands that some *ordinary* foods are an issue for me, and he lets it go at that.
katescarlata
Yes, sometimes we need to help others understand by sharing our personal experience.