In September (2014), I attended a probiotic symposium hosted by Harvard Medical School here in Boston. Leaders around the globe spoke about the changes that occur in our gut microbiome throughout the lifespan.
The talk mostly covered changes in our microbiome rather than what probiotics one should take to aid symptom management for IBS but I will attempt to provide a quick recap of the symposium and add in little bit more…
Oh…and just as a pre-warning….I don’t usually post long posts. This one. Will. Be. LOOOOONG.
Let’s start with some basics:
Gut flora/microbes: We have numerous bacteria, archaea, viruses, and yeast that live inside our gastrointestinal tract. Collectively this group is called our gut microbiome. It’s been suggested that the human body evolved as a vessel for these microbes. Yikes….just think about that!
The gut microbiome includes communities of microorganisms from the three kingdoms of bacteria, yeast, and archae plus viruses that live primarily in the large intestine. The human microbiome consists primarily of bacteria, most of which make their home in the large intestine.
More than 1000 species of bacteria can be found in the human gut microbiota but it’s been estimated that only 150 to 170 predominate in any one person.
Commensal bacteria refers to non-harmful co-existing microbes. Most people harbor some known pathogenic bacteria. But in the right mix, these microbes, that can contribute to health problems, seemingly stay out of trouble…as long as the microbes remain in balance. It appears that food borne illness and infection can disrupt this very important balanced ecosystem and result in functional gut problems–and the condition known as post infectious IBS. Of course, antibiotics can effect this delicate ecosystem of microbes too!
Probiotics are defined as “live microorganisms which when administered in adequate amounts confer a health benefit on the host”-per World Health Organization (WHO).
Prebiotics are food for our microbes–substrates in our diet that provide a health benefit by selectively promoting the growth of beneficial bacteria in the intestine. Some FODMAPs such as FOS, inulin and likely GOS are examples of prebiotics.
Bacteria in our intestine play a big role in health—not all ‘bugs’ are bad!
Microbes help provide energy for cells in our intestinal tract, supporting digestion–they have enzymes we don’t and help our bodies receive and absorb well-needed nutrition, synthesizing vitamins (B-vitamins, vitamin K, folate), educate the adaptive immune system, modify inflammatory reactions in the body, keep the bad bacteria from getting unruly…and so much more… scientists haven’t even scratched the surface yet in this very interesting area of research! I have said it before…and I will say it again….in many ways, our health is in the hands of these microbes!
Breaking research from UNC shows that IBS patients depending on their sub-type–or primary symptom such as constipation, diarrhea, bloating–have different clusters of microbes. i.e. Constipation predominant IBSers will have similar flora clusters compared to other IBS-C patients –and this differs compared to IBS-D patients etc.
So perhaps it makes sense to choose a probiotic based on symptoms. If your primary symptom is bloating and a probiotic has scientific evidence to help with bloating–that might be a better bet than selecting a random probiotic that has been shown to help patients with diarrhea as their primary symptom.
The World Gastroenterology Organisation Global Guidelines Probiotics and Prebiotics can be found here and is a reference I use in my practice when and if I am selecting an appropriate probiotic based on symptoms for my patients. And this is a research article that also discusses what probiotics are indicated based on symptoms.
And we know what we eat, changes our gut microbiome. Here is a review of an animal study–but shows just in 3 or 4 days with dietary changes our flora population changes.
Research involving the gut microbiome is going fast and furious and we are expanding our knowledge about these little critters that live within us. For patients with functional gut disorders, such as IBS, the gut microbiome and alterations, I believe, is a big reason for the alteration in the way the intestine moves. Studies have correlated methane production by microbes in our gut to constipation and even weight gain/higher BMI (body mass index).
So what should an IBS patient to do? Add probiotics to the daily regimen? Add prebiotics, carbohydrate food sources, for their gut bacteria? This is an evolving area and WE really don’t know yet. There is some research in IBS patients showing beneficial symptom reduction with probiotics–but the research is scanty. In my clinical experience working with IBS patients, the most beneficial probiotics have been Align (Bifidobacterium infants 35624), Culturelle (health and wellness formula w/o inulin), VSL#3 and B. animalis found in Activia yogurt. But because we all have our own ‘fingerprint’ of bacteria—and presenting symptoms–it’s doesn’t seem to be a one-size-fits all approach. So I recommend you work with your health care practitioner to select a probiotic based on your medical history and primary symptoms. The use of probiotics for those who suffer with small intestinal bacterial overgrowth (SIBO) is controversial. In my experience working with clients with SIBO, probiotics tend to make symptoms worse rather than better. But…again the jury is out. We NEED more research in this area FOR SURE!!
Okay, now…I will provide some key take aways from the Probiotic symposium I attended at Harvard Medical School:
- The microbiota during pregnancy changes with dramatic shifts in gut and vaginal microbiome with a rise in Proteobacteria and opportunistic pathogens. Research also shows that the placenta has its own microbiome and these bacteria likely seed the baby’s gut prior to birth. We used to believe baby’s were born with a sterile gut which was seeded by the mother’s microbes on delivery. The role in probiotics in pregnancy may change as we learn how they may impact mother and child’s health outcomes during pregnancy.
- Dairy farm living and asthma risk.Diet and microbiotia exposure during pregnancy and in young life was also reviewed looking at children that live on a dairy farm. Exposure to raw milk, contact with livestock & barns seems to lower risk of wheezing, rhinitis, fever and inflammatory markers. {Note: raw milk can contain listeria–which can cause a life threatening food borne illness so I am not suggesting you drink raw milk.}
- Changes in the small intestinal microbiota is associated with greater diabetes risk and obesity. Research presented by a Swedish research team shows that fecal transplants from lean donors can lead to beneficial changes in the recipients microbiota and insulin sensitivity. This science may evolve to include vaccinations or probiotics to combat insulin resistance, obesity and diabetes.
- Gut microbiota and the brain: A number of animal studies reveal the impact of the gut microbiome on emotional behavior and stress. There are multiple ways that the gut microbiome impacts brain signaling–and perhaps the brain then can change the gut micro biome. (The chicken or the egg type scenario) There is a great deal of cross talk between the gut and brain…but most people with IBS already knew that!
- Autism and gut microbiome: GI symptoms are common in those with autism. Animal studies using mice that show brain and behavior features of autism also display autism related GI abnormalities–including alteration in gut microbiome. Research using treatment with commensal bacterium, shifts the microbiome toward that of healthy controls–and this helped improve GI symptoms and autism-related behaviors.
- Prevention of recurrent C. Diff Infection: Clostridium difficile infection has increased 3-4 fold over that past decade. Antibiotics help treat symptoms–but recurrence is common. The intestinal microbiota plays a role in preventing C. diff infection–so the role of probiotics may be key in prevention–but studies in this area have been inconsistent. Fecal transplant has a good success rate for treating recurrent C. Diff infection.
- Microbiota and atherosclerosis: Diet nutrients: choline, phosphatidylcholine and carnitine are acted upon by gut bacteria and can form trimethylamine which is then converted to trimethylamine-n-oxide (TMA0). In animal studies, TMAO is strongly linked with heart disease. Human studies show a high correlation of TMAO with risk of MI, stroke and death.
This science is new and evolving. We have a long way to go…but stay tuned! I think the gut microbiome plays a big role in digestive distress, weight gain, diabetes and more! I provided some details on this science in the New York Times bestseller that I co-authored, 21 Day Tummy, which provides some of this ground breaking science about the gut micro biome, obesity and digestive distress.
How to look for FODMAPs in your probiotic:
The probiotic above has inulin–a FODMAP source.
 This kid’s probiotic (same brand name as the first example)–has mannitol and inulin–both FODMAPs.
This kid’s probiotic (same brand name as the first example)–has mannitol and inulin–both FODMAPs.
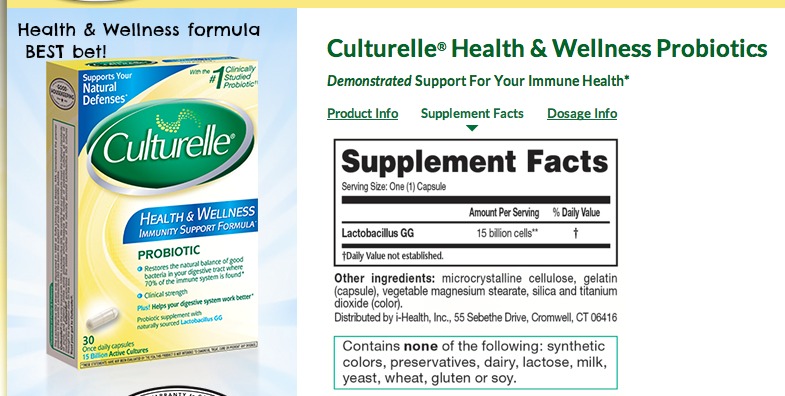 And this version of Culturelle–does not have added FODMAP ingredients. And is suitable on the low FODMAP diet.
And this version of Culturelle–does not have added FODMAP ingredients. And is suitable on the low FODMAP diet.


Beth
so, which probiotic is best for constipation and/or pain???? No name was given that I saw. Thanks so much.
katescarlata
Beth, You should work with your health care provider to figure out which probiotic is most suitable for you. This blog is to provide general information and not personalized care. It is SO important to work with a gastroenterologist and dietitian to provide individual guidance.
Beth
I have gone to 6 different gastroenterologists and not one of them knows anything about treating IBS…they all say to live with it. I think because it’s such a “randomized, undetectable” condition…they don’t take it seriously or put any time into researching how to help it.
Nancy
I also have this question; the charts gave a lot of information (thank you!) but it’s hard for the consumer to know the brands. Any way we can get this info?
Aurelia L.
Thank you for the helpful information! It’s incredible how research can open the doors to so many more questions that can lead to helping our society feel better everyday. Nevertheless, should I look out for any particular ingredients in a Probiotic that may contain high FODMAPs or are any of them okay to take despite the Low-FODMAP diet? I was recommended to try Renew Life Ultimate Flora Critical Care because they are gluten/dairy free, however I was unsure if they don’t contain any FODMAP ingredients. This is the link to the product: http://www.amazon.com/Renew-Life-Ultimate-50-Billion/dp/B001LIW11Q/ref=sr_1_1?ie=UTF8&qid=1413990405&sr=8-1&keywords=ultimate+flora+critical+care+50+billion
Rachel
My GI was anti-probiotic, if you can believe that. Honestly, I think that ingesting too many probiotics led to my first and most painful flare-up of IBS that I’ve had in my life. Taking probiotics with prebiotics as well as drinking Kambucha and eating yogurt daily… I became so bloated and my abdomen was so distended for weeks, I ended up being prescribed 2 different antibiotics, being officially diagnosed with IBS (colonoscopy was negative although endoscopy showed signs of gastritis and acid reflux issues), and being told to avoid probiotics altogether. My GI was supposedly doing clinical trials whereby he posited that probiotics has become overblown due to the fact that it’s now a million dollar industry. He told me to avoid. Afterwards I did the low FODMAP diet for 6-8 weeks under a coaching program (Strands of My Life) which helped me immensely. I still have the probiotics in the fridge but I haven’t dared try them again. Btw, I was never given a SIBO test so I have no idea if that’s the issue. I saw two GIs who really never were able to figure out why this happened to me (and I’m not lactose intolerant nor do I have Celiac’s).
suzanne
Hi Kate, Im so grateful for the ‘internet’ guidance you have given me alongside my fantastic Holistic Doctor i have at last found who seems to know EVERYTHING about digestive issues ( alongside yourself !). After 3 years of struggling with what i thought were more and new food intolerances I have discovered its SIBO and am right now in the middle of treatment. We all have our nightmare stories, mine is a series of events,first a parasitic infection Dientameoba Fragillis and treatment of 3 courses of powerful antibiotics (each combined of 2 drugs), then 3 years of suspected food intolerances, testing for SIBO infection ( wrongly diagnosed as negative by the nurse) then trying to live with the symptoms, another SIBO test and treatment with the wrong antibiotic, my most recent and 3rd SIBO test shows I’m positive and now at last i have hope that it will soon be gone as i am taking Rifaxamin,I’m struggling with the side effects but i WILL NOT STOP TREATMENT 🙂 Your latest post is most timely, i am making sure i have all the information i need to support my plan for healing after finishing treatment and taking a new test. Ive checked my fridge and i already have all the correct probiotics i need! So, thanks Kate once again and my advise to all those out there who are suffering is to educate yourselves with all knowledge you can find on digestive issues and make sure you have all the tests via a knowledgeable Holistic Doctor or equivalent, if you are not satisfied with their knowledge MOVE ON and find another 🙂 and most of all DONT SELF DIAGNOSE, its a minefield. Kind Regards and Good health, Suzanne. x
Joyce
Suzanne, would LOVE to know the name of your holistic doctor, very hard to find a good one (at least here in CT). I also have ongoing SIBO and aside from the Rx (also Rifaximin) prescribed by my regular GI, I really would like to approach this from a holistic standpoint. Can you expand on your wealth of knowledge? Thanks very much!
Samantha
Do you have any thoughts on the growing field of fecal transplants? As someone who had food allergies and FODMAP problems arise suddenly and simultaneously, I’m getting fairly certain that would help me, especially given the recent study linking one particular gut bacterium strain to food allergies. Is there any sign of the medical community advocating this treatment option for anything other than C diff. infections anytime soon?
katescarlata
Samantha, I do believe there is some interest in trialling fecal transplants in patients with functional gut disorders—but not sure if this is actively being studied at this time.
BethB
I agree and commiserate with the other Beth that many/most g.i. docs aren’t helpful for treating IBS, and many don’t test for SIBO, though we can do home tests with a doctor prescription. To be fair, following diagnosis, it’s really more the *knowledgable* RD – and some are not though think they are, ask me how I know – who is better equipped to do long-term food testing and education, like with FODMAPs. That may be a productive search for the Beths like me out there. : )
Doctors aren’t primarily patient educators. It would certainly benefit their patients and enhance their practice to have RDs on board or refer to RDs, however.
Btw, I’m in an area with tons of g.i. docs but recently began driving two hours to see a g.i. doctor at Johns Hopkins, whose passion (his word!) is functional gut disorders, including IBS. I’m also working with an RD. It’s been a long, frustrating journey to find the practitioners who are finally helping me. Don’t give up.
Another Beth
Wendy
Thank you so much for the most interesting article. My problem is diarrhea, which the low fodmap diet has helped immensely. I was saddened to learnt hair probiotics were not effective with this form of IBS. I have been taking Culturelle, but I will now look at the ingredients. Do you think I should continue to take it on a regular basis?
Maree Kniest
Thanks for the post! I have been doing my own research on this stuff for a long time. I have IBS and have been doing low -fodmap for quite some time with some success.
Something i have been wondering:does the type of preparation of the food make a difference? If a food is fermented as opposed to not? If a grain is sprouted or not? Cooked -vs- raw? I know that fermented foods contain beneficial bacteria and am wondering if you know anything about this in terms of IBS? Thanks, Maree Kniest
katescarlata
Maree—see my reply above to Ryan. In addition, sprouting beans does lower the oligosaccharide content. How much, I am not sure. I suppose that depends on how long the beans are sprouted. I love the notion of sprouting seeds, nuts and beans though–as this makes more nutrients available to the body—and most likely aids the foods digestion too. I will be doing a post in December on sprouting. So come on back and read on 🙂 And cooking food vs. eating raw–that can go either way–it can concentrate the amount of FODMAPs and change starch components–it’s a bit variable depending on the food.
Lisa
Thank you for the links to the research. After reading through them I think I have a direction to take regarding specific probiotics. I noticed that your product recommendations did not include a source of b. lactis. Is there a specific reason for this, or is it just outside of your experience?
Thank you for your willingness to share your knowledge with all of us. For the first time in over 40 years I am finding real improvement of my symptoms.
katescarlata
When choosing probiotics, in my opinion, at this point in time, it is best to choose one that has shown demonstrated health benefits. It’s not as simple as just adding more lactobacillus. Bacteria are specialized down to the strain. You can have several different types of lactobacillus acidophilus and all 3 strains will perform differently in the body. So B. lactis–is not enough info. Is it the strain of B. lactis that has been shown to be beneficial in your IBS subgroup? And I imagine–this will be tailored even more to the patient as we identify the type of bacteria we each individually harbor in our intestines–and what needs to be added to derive a particular health benefit. BUT…of course we are not quite there yet. I could go on for 10 blog posts about probiotics–it is very interesting science–and there are more myths out there than truths.
Beth
Lisa, where did you find the information, exactly, to choose specific probiotics for your specific symptoms? Would love some direction that I am missing. Thanks so much. would be greatly appreciated.
Marcy
Dx and treated for SIBO awhile back. Deal with IBS-C – cramping every few weeks that sometimes leads to D. Follow Low FODMAP diet and Dr. Pimentel SIBO diet. Will see ENT tmr for Sinus issues (maybe the microb of sinus related to stomach microb?). I fear needing antibiotics to treat possible sinus infection. GI Dr. suggested taking Probiotics Flora Q & Florastor while on antibiotics to hopefully avoid any side effects. Suggested staying on Flora Q after antibiotics as may help IBS. What are your thoughts on which probiotic to take while on antibiotics. I remember my daughter’s Peds Dr. having her eat yogurt after every dose of antibiotics. Hoping SIBO doesn’t return with Probiotic…I never dealt with SIBO or IBS until after strong antibiotics years ago for sinus infection…How do you handle taking antibiotics if needed? I have tried to fight it off for months now. I did notice the link is from 2011, any changes?
suzanne
Kate, Its quite a concern to know that the different strains of probiotics even have sub groups, just when you think you know about something…. you don’t! I will talk to my Holistic Doctor about this when i have completed my course, Im on day 8 of Rifaxamin today …. pleased to say the side effects eased up nicely after the first 3 days, i presumed i had die off/ Herx reaction as the side effects were pretty bad for a while! Joyce I am in Australia so cannot help you with good Holistic Doctor there, only to say keep searching until you find the right one , also, you can have Skype consultations these days.
tomasz
The articles are great but I agree I have gone to a handful of doctors and they don’t have answers. Unfortunately they give the same responses: probiotics may work for you or cut certain foods out. Perhaps a generic guideline of probiotics for the two main groups would be great. Then we would have something to bring to our doctors as well. Even A nutritionist was giving me useless advice that I already knew. Unfortunate. This blog/site has helped me so much at least if not have answers give me some leads.
katescarlata
Tomasz, I understand your frustration! The science in the area of IBS and the gut microbiome is relatively new–and it’s not a one size fits all approach. There are many factors that play a role in each person’s IBS disorder. SO…the reality is…WE don’t have all the answers yet! The science hasn’t caught up to where we all would like it to be but we are on our way…. Typically when I see an IBS client–I am looking for the many factors that play a role in their symptoms. Most of my clients have multiple issues occurring simultaneously. Gut micro biome alterations–a colonic dysbiosis and/ or SIBO, pelvic floor dysfunction, bile acid diarrhea, fat malabsorption, digestive enzyme deficiencies, motility problem, insufficient acid production, overlapping autoimmune disorder….each patient has their own set of issues. Some of these presenting problems can be addressed and managed with diet and/or medications or physical therapy/biofeedback…. EVERYONE is a bit different—and therefore, needs an individual approach. A certain probiotic may work better for symptoms related to IBS-D but not all patients w/ IBS-D will benefit from it–because not everyone w/ IBS-D has the same cause and the same set of problems. It’s complicated. Working with a doctor that enjoys the work of being a detective and help figure out the cascade of reasons for your symptoms—and understanding how to treat them–is key. And of course, working with a dietitian that understands digestion is equally important.
Marissa
Great summary. Thank you!
dkaj
Kate, I think it would be interesting if they opened up their research to not only dairy farmers but all farm families. I grew up on a farm, and did not have any environmental allergies that I remember. Same with my Dad. As soon as he retired from farming, and moved to the city, he developed environmental allergies at age 65. And, we were outside all the time between planting season and harvest time. If a person looks at the countryside of rural farming communities, each farm will have tree lines around their farm houses to provide a wind barrier, but then you have miles and miles of open country side. In the city, their are multiple trees in almost every single person’s lot. Where we live, river birch trees are very very popular, which is one of the trees people tend to have cross contamination issues with also when it comes to fruits. I only remember one of my friends having environmental allergy issues when I was growing up, now in the city, it seems like almost everyone I know is having enviromental allergy issues, and many kids have inhalers due to allergy induced asthma.
suzanne
Hi Kate After taking Rifaxamin is it ok to re test for SIBO after two weeks, this is what my holistic doctor has recommended . Many Thanks Suzanne.
katescarlata
Hi Suzanne, Typically my clients tend to wait a bit longer–maybe 6-8 weeks or sometimes ONLY if symptoms do not feel fully back to baseline.
Wren
What about Saccharomyces boulardii?
Karen
Do you know of any that are both Fodmap free and vegan?Thanks!