Hello my fellow gut health fans! Today’s topic is about the role of prebiotics and probiotics for individuals with IBS.
Let’s start with a primer on prebiotics and probiotics, shall we?
What’s a prebiotic? In December 2016, microbiology, nutrition and research experts were gathered by the International Scientific Association for Probiotics and Prebiotics to discuss a new definition of the term prebiotic. The panel updated the definition of a prebiotic to: “a substrate that is selectively utilized by host microorganisms conferring a health benefit.” This liberalized the concept of prebiotics to include non-carbohydrate substances including the role of other food components such as polyphenols. Polyphenols are plant-based compounds that include: flavonoids, phenolic acids, proanthocyanidins and resveratrol. Dietary polyphenols can act as antioxidants and have the potential to provide anti-inflammatory, anti-viral and anti-microbial effects in the human body. They are found in plant foods, such as wine, tea, coffee, cocoa, cereal grains, soy, fruits and berries. Oh…some of my favorite foods and beverages! Do you agree? 🙂
Prebiotics by definition are utilized by our gut microbes to enhance health. Other well-researched prebiotic sources, fructans (found in onion, garlic and wheat), inulin (chicory root extract, is added to granola bars, probiotics and more) and galacto-oligosaccharides (found in beans and nuts) are poorly digested carbohydrates (and FODMAP sources). They can trigger IBS symptoms. I think the science of prebiotics for gut health will be important for IBS patients in the near future. I encourage you and healthcare providers to follow this research. It may be possible to slowly increase prebiotic intake in a more tolerable manner to potentially enhance gut health and symptoms by altering the gut microbes in IBS patients. Presently, the data to support using prebiotics in IBS patients is not favorable from a symptom standpoint…but more research is needed. Other prebiotics such as resistant starch or polyphenols may be more tolerable in IBS patients–and I believe should be utilized in the diet as tolerated. For more info on resistant starch read my post here.
As a side note, a recent prebiotic study was done on individuals that suffer with lactose intolerance to assess the benefit in managing GI symptoms. The result showed that adding a prebiotic (a specific galacto-oligosaccharide called RP-G28) individuals with lactose intolerance improved tolerance to lactose. Interesting, right? Study here.
What is a probiotic? Probiotics are “live microorganisms that confer positive effects on the host after oral administration”. Several probiotics strains have shown beneficial outcomes in IBS patients but the research in this area is somewhat difficult to generalize as different studies evaluating the impact of probiotics in IBS have used different symptom scales, different probiotic dosing and species. These different study designs make coming to a final scientific consensus on probiotics in IBS difficult as scientists like to see studies replicated to show that the results are truly reliable and can be put to practice. More on probiotics here.
Probiotics MAY help protect our gut from pathogenic microbes, amplify the tight junctions in our intestine to minimize abnormal intestinal permeability and stimulate goblet cells to produce mucus to enhance our protective intestinal barrier.
There are many misconceptions about probiotics on the Internet. Let’s review a few of these so that you can be an educated consumer.
- Adding probiotics will add good bacteria and get rid of the bad bacteria. Despite what you may have heard, using probiotics is not just about adding in “good bacteria” to get rid of the “bad guys”. The gut microbial environment is quite complicated and in the IBS patient, very fragile. We all house some potential pathogenic microbes–even healthy folks. It’s possible that these potentially pathogenic microbes are necessary for our gut microbial balance. We just don’t know. And science is showing us, probiotic science is just not that simple.
- All live bacteria or cultured food is a source of probiotics. Live cultures used to ferment food may help modify the structure or taste of the food, but do not necessarily offer a health benefit. In some cases, fermenting foods such as cabbage and tea can increase the FODMAP content as in sauerkraut and kombucha; so take note if you are sensitive to FODMAPs. If a cultured food contains LIVE microbes that have demonstrated efficacy as conferring human health benefit, then it would fit the criteria for being a probiotic. (Note: pasteurizing a product can kill off the live organisms and it will no longer offer the probiotic effect). And not all bacteria have probiotic benefits. FYI: A general recommendation to “drink a boatload of kombucha per day” is based on little science.
- Lactobaccillus is a good probiotic to take. Again, it’s not that simple. Microbes are classified by division, class, order, family, genus, species and sub-species. All bacteria from the same genus (e.g., Lactobacillus) do not offer same health benefit. Different species may produce very different effects in the human body, so this generalization should not be presumed. A recommendation to purchase some lactobacillus, is too vague. When selecting a probiotic, it should be genus and species specific such as Lactobacillus Rhamnosus GG (Brandname: Culturelle) or Bifidobacterium infantis 35624 or B. infantis 35624 (Brandname: Align)
- All probiotics need to be refrigerated. Many freeze-dried preparations are quite stable at room temperature. The manufacturers are responsible for providing the number of viable cells in the probiotic supplement for the duration of the product’s shelf life and noting that amount on the product label. Some probiotics need refrigeration–but that does not mean one that does not require refrigeration is less effective.
Selecting a probiotic:
Ideally probiotics should be labeled with the following:
- Genus, species, and strain
- Minimum viable numbers of each probiotic strain at the end of the shelf life
- Suggested dose
- Proper storage conditions for the product
When it comes to prebiotic and probiotic science….you should look at the evidence.
If your healthcare provider recommends a probiotic…your next question should be “has this specific genus and species and/or product been researched and shown to benefit the symptoms and/or condition I am trying to manage?”
Dosage for probiotics is usually expressed as the number of colony forming units (CFU). The dose recommended on the label should be consistent with the research regarding how much of the probiotic is necessary to fit the criteria “confer a health benefit to the host.”
The state of research in the area of IBS and prebiotic and probiotic use, unfortunately, is incomplete. We really don’t have great data to work on making solid recommendations to IBS patients. I have provided a few publication links for your review–should you like to take a closer look.
Here is a meta-analysis published in 2015 on probiotic use in IBS, here.
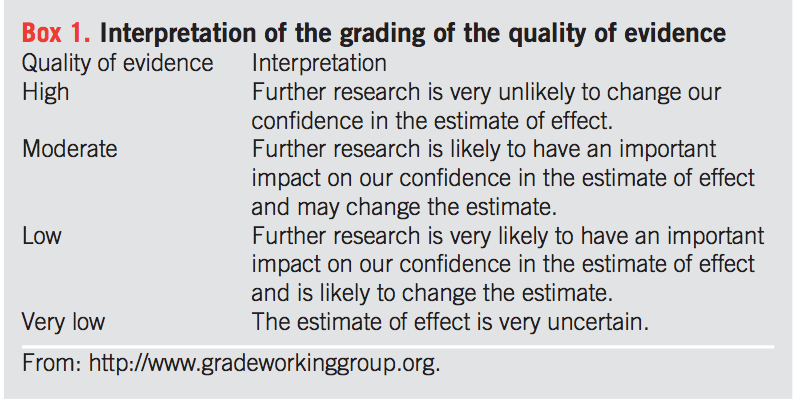
The American College of Gastroenterology Monagraph on the Management of Irritable Bowel Syndrome and Chronic Idiopathic Constipation published in 2014 provides a grading of the quality of evidence for use of probiotics and prebiotics in IBS, here is the “grading” system. Take note of the “Low” and “Very Low” on the chart below.
 Reference: Ford, A et al. Am J Gastroenterol 2014;109:S2-S26.
Reference: Ford, A et al. Am J Gastroenterol 2014;109:S2-S26.
Summarizing the results from this review (see below), you can see that research regarding the use of prebiotics for symptom management in IBS is scarce. This doesn’t mean that all prebiotics will not help IBS symptoms, but rather there is little research at this time. Perhaps with the expanded definition of prebiotics–such as the additional of polyphenols, IBS patients will find certain prebiotics more tolerable and beneficial.
Note, probiotics as an intervention for IBS received a low grade in the 2014 ACG Monograph. As mentioned previously, this is due in part to the fact that most probiotic studies completed in IBS patients used different scores to measure symptom response and a variety of doses and types of probiotics, making interpretation of the benefits of probiotics in IBS less clear. Again, studies should be done a few times to ensure that the information provided is reliable and reproducible–so that we know results just didn’t happen by chance.

Reference: Ford, A et al. Am J Gastroenterol 2014;109:S2-S26.
Although I see variable benefits from probiotics in my clinic where I work with IBS patients, I do believe they are worth a try! Here is the metric I use in practice:
- Select a probiotic with research–not just some random brand at the pharmacy! Sounds obvious…but you’d be surprised.
- Select a probiotic that has been shown to lessen or help manage the symptom I am hoping to address. (i.e. if my patient is experiencing constipation, I would select a probiotic that has research showing it helps manage constipation vs. one that has been shown to help diarrhea.)
- Select the dosing that was effective in the research.
- If the patient is particularly sensitive to oligosaccharides the ‘O’ in FODMAP–I would select a probiotic without these prebiotic additives (inulin, FOS or chicory root)
Here are a few probiotic formulation that have some research to improve common IBS symptoms, albeit, in only a few studies. Check out the resource section at the end of this article for more info.
B. Longum infantis 35624 1 billion CFU per day. Brand=Align may help with constipation.
S. cerevisiae CNCM I-3856 Brand=IbSium 1 capsule 40 billion CFU OR L. plantarum 299v (DSM 9843) 10 billion CFU OR Lactobacillus Rhamnosus GG 5-10 billion CFU (brand name Culturelle) may help with abdominal pain.
L. plantarum 299v (DSM 9843) 10 billion CFU (Brand Swanson L. Plantarum probiotic) may help with bloating.
L. plantarum 299v (DSM 9843) 10 billion CFU may help with incomplete emptying.
L. reuteri DSM 17938 100 million CFU (Brand: BioGaia Protectis Baby Drop formula) may help with constipation due to over-production of methane gas. Research here.
VSL#3 900 billion CFU (multi-strain probiotic) may help with diarrhea. Research here.
Since we all house our very own individual gut microbial fingerprint–at this time, there is no hard and fast way to trial probiotics. The science is just not there yet. Work with your healthcare provider to best guide you in selecting a probiotic–but do realize, we have a way to go before we can make definitive guidelines in this area of potential IBS treatments.
A few more resources to guide you:
Websites for additional probiotic information include: http://isappscience.org/
US Probiotic Guide provides clinical evidence for use of probiotics, brandnames and dosing. (This can be downloaded as an app too).

stephanie
Thank you so very much for this information! It has been so difficult to understand and quantify information on probiotics, and your article is so helpful in understanding why. Many thanks!!
Esther
Super post Kate ! !
Great information !
Thank you for sharing !
Esther
Linda
Have you looked at this probiotic: https://probiogen.com
I found it helpful, it apparently survives the acid in your gut.
Also I have read kefir is better than all supplements.
Loche
Thank you so much for this ! So happy I found your blog. 8 months ago I had an appendectomy, and they messed something up during that surgery and I ended up having another surgery for mesenteric ischemia 3 weeks later ! They took out 2&1/2 feet of my ileum, and illeocecal valve because it was necrotic. I had the c.diff infection from all the antibiotics I was on, and Now I have bile acid malabsorption and pretty sure I have SIBO, cause I can’t even eat any leafy greens (spinach, kale) and I can’t eat any nuts or seeds without running to the restroom within an hour! (Which sucks because I was a vegetarian prior to the surgery). I’ve been trying to get my gut bacteria healthy the natural way….. but it’s a process. Thank you did all the research you do and time you put into your blogs ! You really help so much.
katescarlata
Wow…you really have been through quite a bit. I don’t have an ileo-cecal valve either. A major risk factor for SIBO—so get checked out! Best to you!
Jolie
I started using a probiotic about 5 months ago…I like the results although some may think this is a bit crude: BMs are now a couple times a day (on a good day) larger and better formed (as long as I follow my food rules). This was not the case prior to using the probiotic. I am sold on them and my bum is happier too. = )
katescarlata
Thanks for sharing your experience, Jolie. What probiotic are you using?
Arlene
How long do you typically have a patient use a probiotic? At what point do you suggest they taper off or discontinue a probiotic?
Joe Leech
Hey Kate very informative thanks for this. I will use some of these details to update my own probiotics for IBS post! It thoroughly compares the evidence for the main brands (not random ones), If you haven’t seen it would love to know what you think: https://www.dietvsdisease.org/probiotics-ibs/