Hello Friends! Today’s topic: Resistant Starch. I promised a bit more on gut health topics…so here you go.
What is resistant starch?
Resistant starch (RS), unlike other forms of starch that are digested by amylases (digestive enzymes) in the small intestine, actually ‘resist’ digestion in the upper gastrointestinal tract and thus travels to colon where it is fermented by bacteria, producing important metabolites, including short chain fatty acids (SCFAs) and gas.
Resistant starch is considered a prebiotic fiber. Prebiotic by definition is, “a non-digestible food ingredient that beneficially affects the host by selectively stimulating the growth and/or activity of one or a limited number of bacteria in the colon, and thus improves host health.”
RS intake is associated with reducing blood sugar and improving insulin response in humans, as well as lowering blood cholesterol and triglycerides (blood fat) levels, improving satiety (our feeling of fullness post eating), and reducing fat storage. These positive health effects make adding RS to the diet another way nutrition may reduce chronic diseases associated with high blood fats and insulin resistance such as heart disease (America’s number one cause of death) and type 2 diabetes. But what about gut health?
RS intake may reduce hydrogen sulfide gas production in the intestine. Hydrogen sulfide has been linked with the onset of ulcerative colitis, an inflammatory bowel disease. Hydrogen sulfide is an odorous gas (rotten egg smell) while methane and hydrogen gas also produced by gut microbes are odorless. If you want to learn more about hydrogen sulfide and the GI tract, check out this review. More on hydrogen sulfide, ulcerative colitis and RS later. RS intake also is associated with increasing butyrate, a short chain fatty acid, linked with colonic health.
Where is RS in the food supply:
There are 5 types of resistant starch:
- RSI, type I resistant starch (example: whole or partially milled grains, seeds, and legumes, muesli) Thick outer cell walls of legume seeds and protein matrix of whole grain cereals prohibit water penetration into the starch. Without proper gelatinization and swelling, the starch is unable to be broken down by enzymes.
- RSII, type II resistant starch (example: high-amylose maize starch, raw potato, raw banana starch, green bananas) Cooking alters the starch content, however, and it becomes highly digestible, partly due to starch gelatinization.
- RSIII, type III resistant starch (example: Cooked and cooled starchy foods–think cooked and cooled rice salad or cooked and cooled potato salad). Retrograded amylose has high gelatinization temperatures and cannot be dissociated by cooking.
- RSIV, type IV resistant starch starch with a high level of cross-linking loses the ability to swell during cooking. Consequently, the highly cross-linked starch remains in a granular form after cooking, with little enzymatic susceptibility, and cannot be hydrolyzed by amylases or fermented by microbes.
- RSV, Type V resistant starch (example: Stearic acid-complexed high-amylose starch)
It is unclear whether we can assume that all types of RS offer the same health benefits. More research is needed in this area and is ongoing. Since we all have our own fingerprint of microbes in our gut, likely there will be individual response to adding RS to the diet.
RS types 1-3 are fairly easy to add to your diet such as small amounts of canned chickpeas or lentils, raw oats, green bananas, cooked and cooled potatoes (such as potato salad), cooked and cooled rice or rice pasta salad too. Try different types —adding small amounts and increase slowly for best tolerance. More tips later!
How much do we need?
Individual needs for RS may vary, but most research suggests to aim for a RS intake of 15-20 grams per day. Again, this should be added to your diet slowly for best tolerance. Typically, in my practice, I tend to adjust my patient’s diet to settle gut symptoms down first (often with a low FODMAP diet), then slowly add in RS to the patient’s tolerance. I might start with just 1-2 tablespoon raw oats to start.
The estimated daily intake of resistant starch by Americans is ~5 g per day, much less than the minimum of 6 g of resistant starch per meal recommended for health benefits. [Ref: Murphy MM, Douglass JS, Birkett A. Resistant starch intakes in the United States. J Am Diet Assoc. 2008;108:67–78. ]
One study showed a further reduction of resistant starch intake on the popular Paleo diet compared to traditional diets which is already suboptimal in this fiber. This serves as a reminder that when we alter our diets– healthful nutritional components can take a hit. This is one of the reasons, the low FODMAP elimination diet is recommended as a short term intervention. The goal of the low FODMAP diet is to minimize symptoms but also to help you identify your personal triggers. By doing the reintroduction phase of the diet, you hopefully will learn what foods you can safely add back to your diet without symptom exacerbation. Restricting your diet unnecessarily is not only NO FUN…it can be unhealthy in the long term. Just as an FYI, I will be doing a webinar on the reintroduction process on Feb 9, 2017 with Gastro Girl, learn more here!
Here you will see some of the ways I try to boost my RS intake. I make energy bites with uncooked oats and top my smoothies or smoothie bowl with raw oats and seeds. I also add canned chickpeas to salads and soups, such as in this vegetarian stew.
 Jane Muir, PhD, Head of Translational Nutrition Science in the Department of Gastroenterology, Central Clinical School, Monash University, a biochemist and resistant starch expert, provides some key points about resistant starch, “Resistant starch is a special member of the indigestible carbohydrate family. It does some things in the gut really well but it does not do everything! Resistant starch is now considered by many (who work in this area of science ) to be a ‘prebiotic’ type of fibre- it selectively stimulates the growth of certain bacteria that are able to ferment the resistant starch to produce a short chain fatty acid called butyrate. Butyrate is the major source of energy used by the cells that line the bowel. Butyrate has a number of important effects relevant to the health of the bowel.”
Jane Muir, PhD, Head of Translational Nutrition Science in the Department of Gastroenterology, Central Clinical School, Monash University, a biochemist and resistant starch expert, provides some key points about resistant starch, “Resistant starch is a special member of the indigestible carbohydrate family. It does some things in the gut really well but it does not do everything! Resistant starch is now considered by many (who work in this area of science ) to be a ‘prebiotic’ type of fibre- it selectively stimulates the growth of certain bacteria that are able to ferment the resistant starch to produce a short chain fatty acid called butyrate. Butyrate is the major source of energy used by the cells that line the bowel. Butyrate has a number of important effects relevant to the health of the bowel.”
Butyrate is fuel for the cells of the colon and linked with reducing colon cancer risk.
For a list of resistant starch rich foods, a great reference from my dietitian colleague, Jill Weisenberger, can be found here.
RS for the FODMAPer
Specific to the FODMAPer, the following low FODMAP foods may be good options to boost RS:
Note: portion limits for some foods for FODMAPers are in parenthesis
- Try brown rice salad–cook and cool rice and create a rice salad with low FODMAP veggies, lemon juice, mustard and olive oil.
- Add millet to your diet via millet salad or millet bread. This low FODMAP millet salad looks GREAT!
- Incorporate lentils (limit 1/4 cup cooked or 1/2 cup canned). Try my lentil pilaf recipe!
- Top your smoothies with raw oats (I recommend starting with 1 tablespoon at first).
- Try no bake energy bites with oats! Try my almond cranberry energy bites…so good!
- Add chickpeas (1/4 cup canned) to your salad or soups.
- Cook up sweet potato, cool, and slice in bite size pieces…toss into salad ingredients (limit to 1/2 cup).
- Enjoy potato salad–simple dress in vinegar and olive oil dressing. Garnish with chives!
- Select less ripe bananas to add to your diet. Slice up and add on top of your rice cake or morning oats.
- Cook up some GF pasta salad, cool it down and eat cold.
Be on the lookout for products marketed with high RS–this is an area of interest in the research and as you well know, food companies follow these trends. 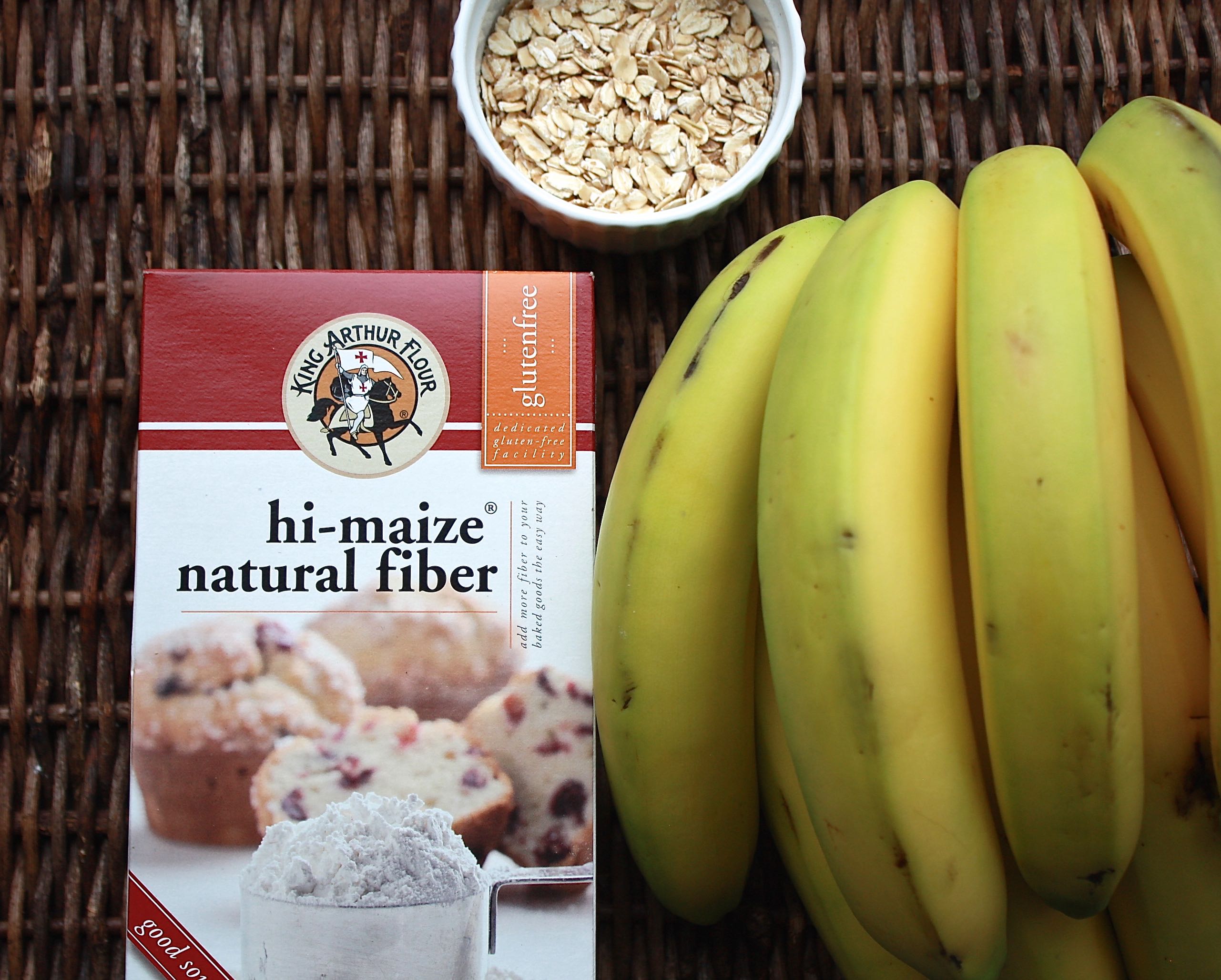
High Maize natural fiber can be purchased via King Arthur Brand and Edward and Son’s has a green banana flour product too that contains copious amounts of RS. Don’t be overzealous with adding RS products or you could aggravate GI symptoms!
EA Stewart from the Spicy RD Nutrition just posted a recipe, Happy Belly Green Banana Flour Brownie Bites that looks amazing using the green banana flour by Edward and Sons, check out her recipe here.
Eat a variety of fibers! RS is good but not the only fiber we need!
Modern day food processing has stripped away much of the resistant starch from our food supply. Dr. Muir notes, “Resistant starch is low in highly processed starch-containing foods. This is why we are getting less in our diet. Resistant starch is found in starch-containing foods. It is particularly high in legumes/pulses, rye, barley and also firm bananas.”
For normal laxation, we do require some bulk to your bowel movements. Dr, Muir, stresses, “Resistant starch is NOT a great bulking agent, and so, has only modest effects on fecal transit and fecal bulk (ie. laxation). To bulk stool, you will need other types of ‘fibre’ in your diet to do this.”
Note to self: a variety of foods and fiber sources should be included in a healthy diet, of course, to your personal tolerance! Slowly upping the fiber in your diet would likely be the route to go rather than added a boatload at once! Also, be sure to include adequate fluids in your diet while you slowly increase fiber for best tolerance. Fruits and veggies, oats, and wheat bran (for those who can tolerate it), contain great bulking fibers.
Role of Gut Microbes in RS Fermentation
Of course, when food is not digested in the upper GI tract, than the gut microbes will likely be involved in its degradation. The process of fermenting resistant starch in our gut results in gas (methane, hydrogen and carbon dioxide) as well as short chain fatty acids, such as acetate, propionate, butyrate and valerate.
Three major phyla, Firmicutes, Bacteroidetes, and Actinobacterium, which account for 95% of total mammalian gut bacteria, are involved in starch fermentation.
Understanding which microbes and their function related to RS fermentation is important for understanding health outcomes associated with RS. We know that microbes can reduce harmful metabolites, including bile acids, phenol, and ammonia, and influence dietary fat metabolism, which influences obesity, colon cancer risk and likely more. A fiber rich diet has been associated with colon cancer risk reduction. Resistant starch is gaining more attention of late as a possible dietary component that may be a key player in colon cancer and inflammatory bowel disease prevention.
(ref: Higgins JA. Resistant starch: a promising dietary agent for the prevention/treatment of inflammatory bowel disease and bowel cancer. Curr Opin Gastroenterol. 2013;29:190–4.)
Nutritional change can result in rapid shifts in our gut microbes. What we feed our microbes is important as is what microbes inhabit our gut. If our gut microbes have the ability to digest RS (ie carry the digestive enzymes to break it down) and are also capable or producing butyrate, then by eating more RS we may be giving them a growth advantage. Because the microbes in our gut rely on each other, by-products of resistant starch fermentation can be used by other classes of bacteria to enhance their abundance through metabolic cross-feeding. Yes, the gut microbiome is a complex ecosystem and really one in which we truly are in the infancy of understanding.
We often associated FODMAP sources, oligosaccharides (wheat, chicory root fiber/inulin) as the primary prebiotics but resistant starch, is a prebiotic too and one that may be better tolerated by FODMAPers.
The Hydrogen Sulfide and RS Connection
CK Yao, a Monash University researcher talks about her recent research, “I showed in our laboratory experiments using human fecal microbiota that resistant starch and fructans actively and effectively suppressed hydrogen sulfide gas production by 50-70%. Hydrogen sulfide which is usually a by-product of really high sulfur-protein (or animal protein) intake (e.g. if you are body building and consuming a high protein diet + supplementing with whey protein). Both carbohydrates (RS and fructans) are rapidly broken down and so we think they do so by shifting fermentation away from proteins.”
Bacteria tend to prefer carbohydrates as their primary fuel but if it is not present in the colon then will ferment protein. Unfortunately, the by-products of protein fermentation tend to have negative consequences in the gut. This is why I alway encourage a balanced meal with both carb and fibers and protein, plus fruits, veggies and healthy fats! Here is a handout to guide you!
For further info check out this article, which highlights hydrogen sulfide gas, how changing your diet might reduce this odorous gas. Interesting to note: psyllium fiber, that found in Konsyl and Metamucil products also reduced hydrogen sulfide gas emissions.
And do remember, when it comes to nutrition and our gut microbiome, many factors play a role.Your colon contains a vast number of microbes and this ecosystem is fragile. We don’t know if adding indiscriminate amount of one type of fiber or copious probiotic bacteria at once is more harmful than beneficial! Even red wine, full of polyphenols, can have a potential positive impact on the gut microbiome increasing probiotic bifodobacteria, but we know too much alcohol in our diet is not beneficial to our liver. Like most things in life (and gut health) its about finding the right amount that works best for you.

Megan King
THIS is a great post! Love the science-y stuff. Keep it coming 🙂
Casey
Thank you for this, Kate! I always learn so much from you.
Esther
This post is amazing !
Thank you Kate …
Corey Cherkas
I just have to say how much I love your blog and your recipes. It is my go to website every day. Today I made the vegetarian stew, but wanted to add so protein so I browned lamb in GF flour and sauteed in Garlic Infused oil, added to the soup, and cooked in crock pot. It tastes delicious. I’m inspired every day, and love having your blog as a trusted resource for this FODMAP journey. Thank you, thank you, and thank you!!!
katescarlata
Awww….thanks you so much for your kind words, Corey! And glad you liked the stew!!
Rhonda Witwer
Great article Kate. You did a good job explaining the topic. I thought you might be interested to know the latest – in December, the FDA approved a qualified health claim that resistant starch from high amylose corn reduces the risk of type 2 diabetes. It was based on 9 clinical trials showing that RS significantly improved insulin sensitivity. This is the benefit I am most excited about, given that 83 million Americans are prediabetic. It is amazing to think that our blood sugar control comes from our guts! For more information, visit http://resistantstarchresearch.com/posts/fda-announces-health-claim-for-resistant-starch/.
However, out of the 139 published clinical trials on resistant starch, there is not consistent data supporting that resistant starch lowers cholesterol. Some studies suggest that it impacts triglycerides, but it is not consistent. If someone wants to lower cholesterol, they are better off consuming viscous fibers such as beta-glucan from oats or barley. FYI – scientists recognize three major mechanisms of dietary fiber’s benefits – bulking (cellulose, soy fiber and others that simply absorb a lot of water but are not fermented or broken down), viscous (thickens the intestinal contents, slowing down cholesterol and sugar absorption and minimizing re-absorption of bile acids), and fermentation (consumed by the microbiota, changing expression of hundreds of genes within the large intestine). You are absolutely correct that we need all 3 types of fibers because they do different things.
Thanks again for a great article.
katescarlata
Thanks for sharing! Always great to learn more from one another!
Tara | treble in the in kitchen
Thanks for sharing so much information, Kate! Portion size is so important (and I feel like it changes from day-to-day, week-to-week! depending on life’s stresses). Saving this for later reference!
Annie
Very timely for me, I have just realised that I fon’t tolerate resistant starch at all. But I cannot find any information on how to avoid it. In your research did you find any helpful info? My problem lies not in the high resistant starch foods, like tapioca starch, plantain flour, green bananas, etc, but the ones that they don’t deign to mention, but which have moderate levels (like ripe bananas), hot potatoes, etc. For example, while I tolerate a corn cereal, frying corn masa made me incredibly sick, possibly through formation of type V RS.